Jump to
Book a visit
$25 typical copay
$100 without insurance
Get expert care for your pain today.
Chronic pain can feel isolating, but finding the right help doesn’t have to. Whether you’re dealing with back pain, nerve pain, or something that hasn’t even been diagnosed yet (been there), there are trusted providers who can help you take control again. Here’s how to find a specialist who understands your pain, offers more than just medications, and perhaps best of all, actually listens.
Hey, we get it: Living with pain day after day is exhausting. It’s more than just physical discomfort; it’s a steady grind that wears down your sleep, mood, and ability to enjoy your life. If you’ve caught yourself googling “pain management near me,” you’re not alone—and you’re totally right to want real answers, fast.
This is your real-world guide to finding care that actually helps, whether that’s a local provider, a virtual pain specialist, or a team that (finally!) takes your pain seriously. Ahead, learn which specialists treat which types of pain, what red flags to avoid, and why the best treatment plans offer more than just prescriptions.
Understanding pain management: what it is and who it’s for
Pain management is specialized medical care focused on reducing and controlling chronic or severe pain. Why? So you can get back to functioning, sleeping, and feeling like yourself again, of course! Conditions like arthritis, rib pain, nerve pain, fibromyalgia, and chronic headaches can all require pain management.
Most types of pain fall into one of three main buckets. These categories help chronic pain doctors understand what’s driving your pain, and guide which treatments might actually work:
- Nociceptive pain: This is the kind of pain you feel from a clear injury or inflammation (think sore joints, a sprained ankle, or post-surgical pain).
- Neuropathic pain: This pain comes from damage or irritation to nerves. It often feels sharp, burning, or like pins and needles. Conditions like sciatica or diabetic nerve pain fall into this category.
- Nociplastic pain: This one’s trickier. It’s real pain, but it doesn’t stem from visible injury or nerve damage. Instead, it’s caused by changes in how the brain and nervous system process pain signals. Fibromyalgia is a classic example.
Types of pain management specialists
Pain care is a multidisciplinary field, meaning the best treatment often comes from a team, not just one provider. Teamwork makes the dream work, right?
“Pain specialists range from anesthesiologists doing injections to physiatrists focused on function, neurologists for nerve-related pain, and even integrative MDs using lifestyle-based care,” says Marjory Bravard, MD, a hospital medicine physician and co-founder of General Medicine. “It’s not one-size-fits-all.”

Types of pain management specialists
Here’s a breakdown of the experts who might be part of your care:
- Pain medicine physicians: These are doctors—often trained in anesthesiology, physical medicine and rehabilitation, or neurology—who specialize in diagnosing pain and overseeing a full treatment plan.
- Interventional pain specialists: Usually anesthesiologists with additional training, they focus on procedures like nerve blocks, epidurals, or spinal cord stimulators—treatments designed to target pain at its source.
- Physiatrists (physical medicine and rehabilitation doctors): These specialists focus on restoring function, especially after injury or surgery. They often lead rehab-based plans and coordinate care with physical therapists.
- Physical therapists: Physical therapy helps you move better and hurt less through hands-on care and guided exercises. PTs can be especially beneficial for managing chronic back pain, joint issues, or injuries.
- Neurologists: These are the go-to specialists for pain related to the nervous system, like migraines, trigeminal neuralgia, or diabetic neuropathy.
- Integrative doctors: Licensed MDs or DOs who combine conventional treatments with evidence-based complementary approaches such as nutrition, mindfulness, and movement therapies to manage chronic pain over time.
Key factors to consider when choosing a pain clinic near you
Not all pain clinics are created equal. Some offer comprehensive care, while others might rush you through a 10-minute visit and send you home with a prescription but no plan—yikes. The difference matters, especially when you’re dealing with something as life-altering as chronic pain.
Here’s what Dr. Bravard recommends looking for when sizing up your options:
- Specialty match: Your pain is unique, and your provider should understand it inside and out. Whether it’s nerve pain, joint pain, headaches, or post-surgical recovery, look for a clinic that actually treats your kind of pain.
- Treatment range: It should go without saying, but one-size-fits-all doesn’t work when it comes to pain. Great clinics offer a toolbox of options, including medications, physical therapy, injections, nerve blocks, and behavioral or lifestyle-based therapies. The more tools, the more tailored your care.
- Doctor qualifications: Make sure your team includes board-certified pain specialists, such as anesthesiologists, physiatrists, or neurologists. This isn’t the time to settle for “general experience.”
- Patient reviews: Go beyond the stars. Read what people say about communication, compassion, responsiveness, and whether they felt heard by a provider. “Look for someone who actually communicates like a human, not just a procedure machine,” says Dr. Bravard.
- Access and convenience: Can you get an appointment without waiting months? Is telehealth available? Are they in-network with your insurance? Pain doesn’t wait, so neither should your care.
How to find a pain management doctor near you
Finding the right pain doctor can feel daunting. But it doesn’t have to. Here are Dr. Bravard’s recommendations to skip the guesswork and get you closer to real relief:
- Start with your primary care provider: Your PCP knows your medical history and often has connections with trusted specialists. Ask for referrals, especially to clinics that treat your specific type of pain.
- Check your network: Already know what type of pain specialist you’re looking for? Use your health plan’s directory or another marketplace. Make sure the provider you choose is in-network with your insurance; it saves you time, money, and billing headaches later on.
- Look at hospital- or university-affiliated clinics: These often have multidisciplinary teams—pain doctors, physical therapists, psychologists—all working together to create a plan that actually works.
- Don’t forget telehealth and other options: If your local clinic is booked, comprehensive virtual care can get you started fast. You’ll talk to board-certified providers who can evaluate your pain, suggest next steps, prescribe medications, and coordinate care with specialists.
Don’t have a PCP? Need telehealth or a comprehensive marketplace to choose a provider? No problem—General Medicine’s got you covered with accessible, personalized care.
Bottom line: Finding the right pain doctor is about finding smart leads, doing a little homework, and knowing what good care should look like.
Spoiler: The best care for you won’t look just like everybody else’s.
Questions to ask a potential pain management doctor
Before you commit to a provider, it’s worth asking a few key questions. Think of it like interviewing someone for an important job—because this is one! You want a doctor who not only has the right credentials, but also treats you like a partner in your own care.
“Ask how they typically approach pain like yours, what treatments they use beyond meds, and how they work with other providers,” says Dr. Bravard. “It’s a great way to sniff out philosophy and fit.”
Here are some specific questions to help you gauge overall fit:
- How do you typically treat pain like mine? This helps you determine if they have real experience with your condition or if they’ll take a generic approach.
- Do you offer non-opioid or integrative options, like physical therapy, injections, or mind-body strategies? The answer can tell you whether they lean on quick fixes (like medication) or believe in treating the whole person.
- What’s your philosophy on long-term medication use? This question is especially important if you’re concerned about dependency, side effects, or simply want a more sustainable plan.
- Will you collaborate with other specialists or therapists? Chronic pain often overlaps with other health conditions. A team-player mindset is a must.
If their answers feel vague, dismissive, or overly focused on prescriptions alone, keep looking. The right pain specialist will respect your questions and your experience.
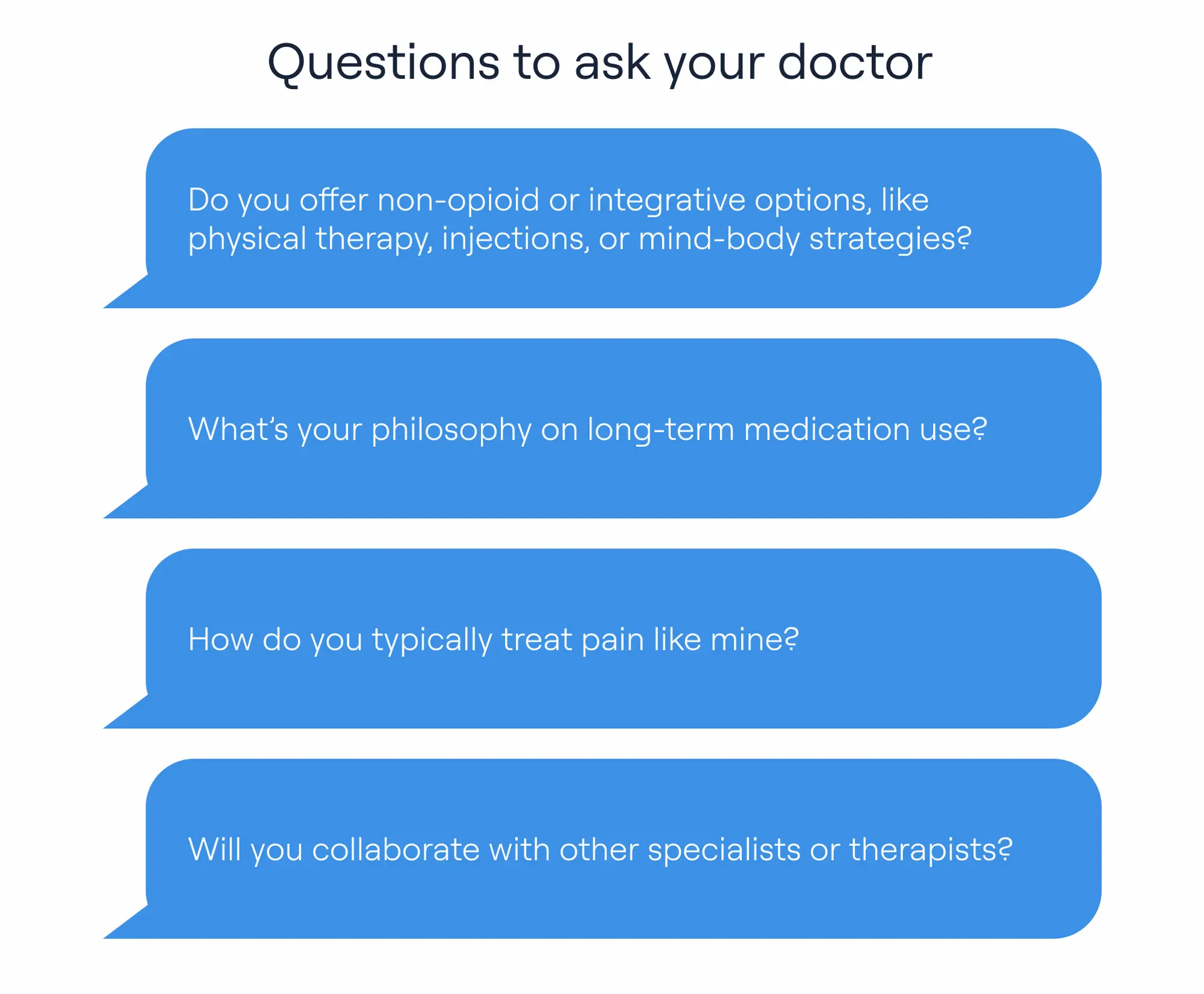
Questions to ask your doctor
Red flags to watch out for when choosing a clinic
Unfortunately, not every pain clinic is created with your best interests in mind. Some lean on outdated methods, offer one-size-fits-all plans, or push medications without looking at the bigger picture. Here are some red flags that should give you pause:
- An immediate push toward opioids: If a potential doctor recommends opioids as the go-to solution, that should raise some alarms for most non-cancer chronic pain. Exceptions include acute injuries, post-surgical pain, or advanced cancer, where opioids may be appropriate early but should still be part of a broader treatment plan. While opioids can be part of a thoughtful plan, they should never be the only tool on the table.
- Clinics promising “quick fixes” or miracle cures: Chronic pain is complex. If a clinic says they can solve it in one visit or guarantees results, be skeptical.
- A lack of credentials: If the clinic or doctor you’re considering doesn’t have experience with your type of pain, they’re probably not the best option for you.
- Doctors who don’t explain their process or listen to your concerns: You deserve a provider who takes the time to walk you through your treatment plan and considers your goals, not just the clock. “If they operate like a high-volume clinic that rushes visits without tailoring care, that’s your cue to keep looking,” says Dr. Bravard.
Benefits of virtual pain management visits
When your body hurts, the last thing you need is a broken system. Virtual care in general has changed the game, especially for people in rural areas, busy caregivers, or anyone juggling multiple responsibilities (like you).
With virtual pain management visits, you can:
- Access board-certified providers from home: When you’re in pain, even getting out the door can feel like a chore. Virtual care removes that barrier so you can get expert help from home. Some procedures, imaging, and physical examinations still require in-person visits, but virtual care can start the process and coordinate those as needed.
- Easier access to specialists: You shouldn’t have to drive two hours to see someone who understands your condition. With telehealth, distance isn’t an issue. You can connect with pain specialists who might otherwise be out of reach.
- Reliable, ongoing support that actually fits into your life: Showing up for virtual check-ins is way easier than rearranging your entire day for an in-person appointment. That means you’re better able to follow through, stay on track, and get comprehensive, coordinated care.
Benefits of virtual pain management visits
The takeaway
- Knowing whether your pain is nociceptive, neuropathic, or nociplastic helps guide which treatments and specialists are the best fit for you.
- Anesthesiologists, physiatrists, neurologists, physical therapists, and integrative doctors all play different roles, so pick one that fits your needs.
- When you’re shopping around for a specialist, ask clear, targeted questions. A good provider will walk you through your options, explain their approach, and coordinate with other specialists if needed.
- Watch for red flags. If a clinic pushes opioids right away, offers “quick fixes,” or doesn’t take time to explain your plan, keep looking.
- Telehealth can give you faster access to board-certified pain experts without the travel or long wait times.
General Medicine follows a strict editorial process, including using real experts to write our articles, vetted primary sources, fact-checking, a secondary medical review, and updates as necessary. This article was medically reviewed and fact checked by Swapna Ghanta, MD, and Ecler Ercole Jaqua, MD.
Frequently asked questions (FAQs)
What qualifies you for pain management?
If you’ve been living with pain for more than three months—especially if it’s not responding to basic treatments like rest, over-the-counter meds, or physical therapy—you likely qualify for pain management, says Dr. Bravard. This includes pain from injury, chronic illness, surgery, or unknown causes that interfere with your daily life.
When does chronic pain become too much?
Chronic pain becomes “too much” when it starts to affect your sleep, work, mood, mobility, or relationships. If it’s interfering with daily functioning or your mental health, it’s time to seek specialized care.
What are the three types of pain management?
According to Dr. Bravard, pain management typically involves three main categories (and many treatment plans combine some or all of them):
- Medications: These include anti-inflammatories, nerve pain medications, and muscle relaxants.
- Procedures: Nerve blocks, injections, and electrical stimulation are common pain-relief procedures.
- Rehab and behavioral therapies: Physical therapy, mindfulness, and cognitive behavioral therapy can all help ease pain.
What is the most effective pain management?
The most effective approach is personalized and multimodal, meaning it uses a mix of strategies based on the type and source of your pain. This might include medications, movement-based therapy, procedures, and mind-body techniques.
What is the best therapy for pain management?
There’s no single “best” therapy. Ultimately, the best treatment (or treatments) for you depends on your pain type.
What is a common medication used for pain management?
It depends on the cause of your pain. Common options include NSAIDs (like ibuprofen for inflammation), SNRIs (like duloxetine for nerve pain), and anti-seizure medications (like gabapentin or pregabalin) for neuropathic pain. In some cases, doctors may prescribe opioids, though these are used cautiously and usually only when your pain is severe and other treatments haven’t worked.
Our editorial standards
At General Medicine, we cut through the clutter to make health care clearer, faster, and easier to navigate. Every article is grounded in evidence-based research and peer-reviewed journals, reviewed by medical professionals, and written in accessible language that helps you make health decisions with confidence. We’re committed to ensuring the quality and trustworthiness of our content and editorial process by providing information that is up-to-date, accurate, and actually useful. For more details on our editorial process, see here.




