
Jump to
Book a visit
$25 typical copay
$100 without insurance
Get a legitimate doctor's note online today for work or school.
So you’ve got a cough that’s been dragging on, eh? But you’re not sick with the flu, the common cold, or another infection. What could it be? A pesky and persistent cough could be a sign of an underlying condition or something in the environment triggering airway irritation. Read on for some common culprits.
I wish I had a wheel I could spin, like a casino game of roulette, and it would land on the correct answer to my medical questions. “What is this cough all about? Am I getting sick? Is it smallpox?” Okay, kidding about that last option.
For some people, a cough is an obvious sign that they are coming down with something, such as a cold, the flu, or another virus or bacterial nasty. But for others, like me, I also wonder whether I’m having an asthma or allergy flare (hello, pollen, my old frenemy) and need to tweak my care routine. Plus, several other issues can cause a persistent or chronic cough, even when you’re not sick with an acute infection. Air pollution surges, such as during wildfire season (which is getting longer, by the way) come to mind.
In this article, we’ll cover reasons for a persistent cough that won’t go away when you’re not sick, persistent cough and chronic cough causes (including how these are different), and more.
Understanding chronic or persistent cough
Any ongoing cough is a persistent cough, meaning it hasn’t gone away even though you’ve tried to break up with it. But persistent coughs get categorized by their duration. Here’s how that breaks down by timeline:
- Acute cough: a persistent cough lasting less than three weeks
- Subacute cough: a persistent cough lasting three to eight weeks
- Chronic cough: a persistent cough lasting longer than eight weeks
Sometimes a cough can show up before you notice other signs of illness, such as during a bout of the common cold or flu. Think of it as one of the first guests to arrive at the party, before body aches and fever show up. (I don’t know about you, but I’d like to disinvite myself to this shindig.) Other times, a cough can linger after the rest of your symptoms have resolved. It can be the guest who refuses to leave even after you’ve cleaned up and begun turning off the lights.
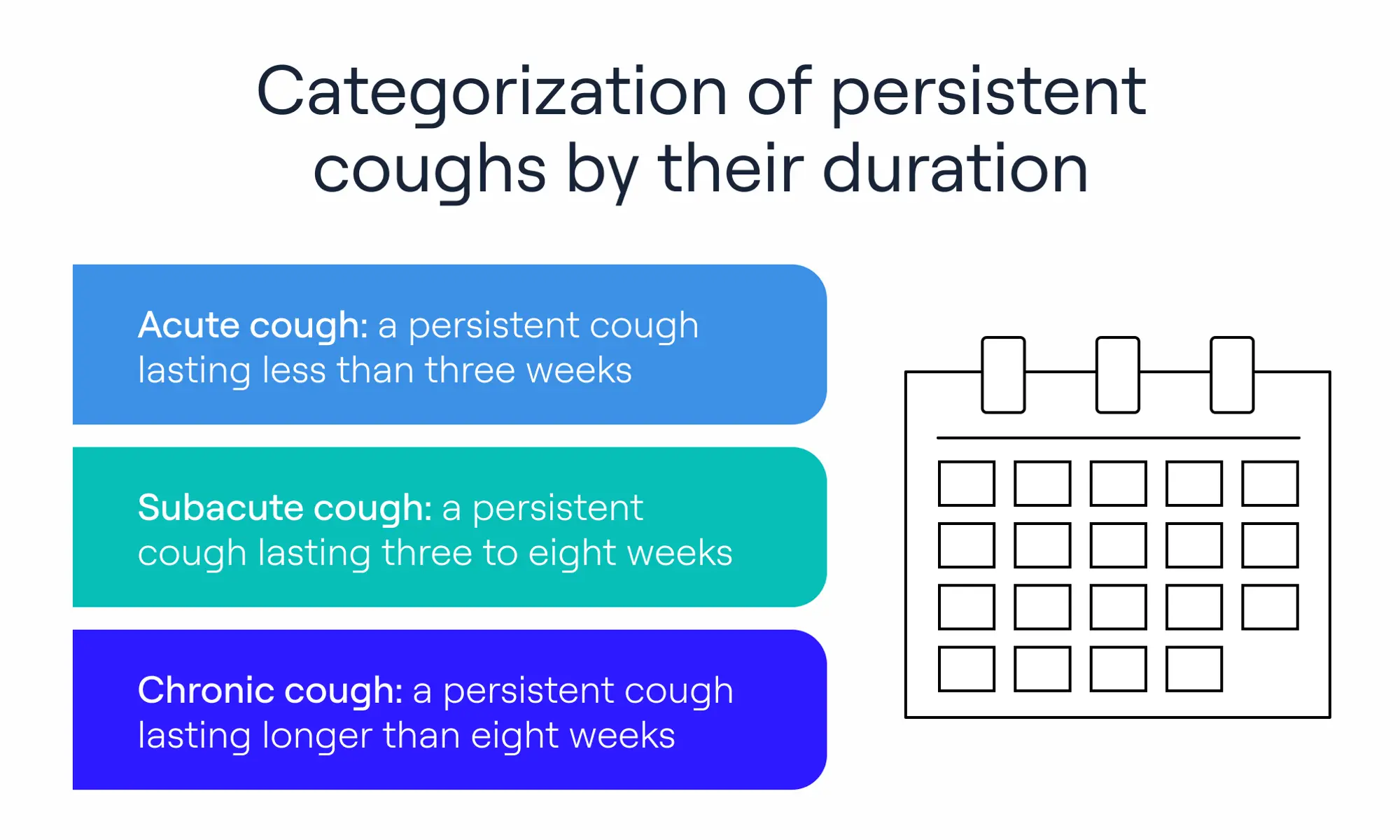
Categorization of persistent coughs by their duration
But a cough doesn’t have to mean you’ve got, or had, an infection. Sometimes a cough will persist for other reasons, and knowing about them can help you decide next steps and remedies.
Common causes of a cough that won’t go away (When you’re not sick)
Now let’s explore some common causes of persistent coughing, along with some uncommon ones to cover the most bases.
Postnasal drip
As an allergic gal, I’m well acquainted with upper airway cough syndrome, more commonly called postnasal drip, which is when thickened nasal secretions drain down your throat (mmm!), often causing a tickle where you definitely don’t want tickles. The issue can lead to a cough, excessive throat clearing, halitosis (bad breath) and a sore throat that worsens upon swallowing.
Common contributors include allergies, sinus infections, and irritants. Less commonly, structural factors like a deviated septum, when the cartilage that separates your nostrils is crooked, narrowing one of the passages. This may play a role by impairing drainage of mucus.
Mucus is a normal part of life, with glands in our throat and nose producing it constantly to clean our nasal passages of debris and pathogens and to moisten the air we breathe in. We swallow mucus mixed with our saliva without really noticing it. But sometimes it thickens and causes that sensation of mucus sticking around, dripping down your throat from your nose.
Triggers include illness, allergies, dry air, hormonal changes (including during pregnancy, the menopausal transition, and while taking hormonal contraception), spicy foods, changing weather, strong odors, some medications (including those for high blood pressure and birth control) and even bright lights. (Just one of the many reasons I live like a vampire and shun any sort of overhead lighting.)
Keep in mind that postnasal drip can be subtle, and you may not realize that it’s causing a cough. That’s because it doesn’t always have a clear trigger, such as allergies or a sinus issue.
Gastroesophageal reflux disease (GERD)
Gastroesophageal reflux disease (GERD) can cause GERD-related chronic cough (aka GERC, for those who love a fun acronym). GERD occurs when your stomach contents reflux into the esophagus (your food pipe), irritating the lining. This irritation can trigger a reflex that activates cough receptors in the airways, even if liquid never enters the windpipe itself, and which can contribute to a not-so-fun hacking cough.
Kara Wada, MD, the founder and CEO of Immune Confident Institute, describes the two ways GERD can cause GERC. “Liquid from the stomach can sneak into your windpipe and irritate the nerves in the airway triggering a cough,” she says.
“Nerves in the esophagus and windpipe communicate with one another,” she adds. “Irritation from the stomach contents in the esophagus can inadvertently trigger the cough receptors almost like a car alarm that is overly sensitive.” Unfortunately, in the case of GERD, you can’t just grab your key fob and shut the thing off. But effectively treating GERD, whether with diet or medications, can help.
Asthma or reactive airway disease
I was diagnosed with asthma as a toddler, so I know all too well how it can trigger a cough during exacerbations or when undiagnosed. A cough was one of the reasons my mom hauled me to the doctor in the first place to get checked out. I’ve been a rescue inhaler-carrying member of the asthmatic club ever since.
Reactive airway disease is a term, rather than a condition, to describe asthma-like symptoms where the cause is unknown. Sometimes it crops up after an infection, such as respiratory syncytial virus (RSV) or bronchiolitis. RSV is a common respiratory virus that tends to cause more severe symptoms in young children and older adults. And bronchiolitis is a lower respiratory tract infection that RSV can cause.
Chronic obstructive pulmonary disease (COPD)
Chronic obstructive pulmonary disease (COPD) is an umbrella term for several lung diseases that cause airway inflammation and damage that can restrict airflow, which often leads to a cough. The two main types include chronic bronchitis, defined by a productive cough lasting at least three months in two consecutive years, and emphysema. Both are usually related to smoking or environmental exposures, though infections can worsen symptoms.
Although smoking is a common cause for both, other causes include exposure to secondhand tobacco smoke, chemicals, or cooking or fireplace smoke (that’s not properly ventilated). Additionally, some people lack the alph-1 antitrypsin protein, which protects the lungs from damage. In this case, a person can develop emphysema without these exposures.
Heart-related conditions
If you think of your body as a town, you know that your heart and lungs are pretty much direct neighbors, and issues with one can affect the other. (Just over here giving side-eye to my neighbor who leaf-blows his yard refuse into mine. Sigh.)
The most common cardiac cause of chronic cough is congestive heart failure. This does not mean the heart is literally failing (although it’s a scary term), but rather that fluid has built up in the lungs, causing irritants and leading to a cough. Other heart conditions, such as cardiomyopathy (a disease of the heart muscle) heart valve diseases, and arrhythmias (irregular heartbeats) may contribute indirectly to a chronic cough by worsening fluid overload.
Medication side effects
Your cough culprit could be in your medicine cabinet or pill case. Some medications can cause a cough as a side effect. These include:
- ACE inhibitors to treat high blood pressure and some heart conditions
- Beta blockers to treat high blood pressure and some heart conditions
- Nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen, often used as pain relievers
- Statins to combat high cholesterol
- Methotrexate, a disease-modifying antirheumatic drug (DMARD), prescribed for rheumatoid arthritis and certain cancers
If you suspect your cough is a medication side effect, talk to your prescribing physician or another doctor right away.
In certain instances, the cough could be a sign of bronchoconstriction (airway narrowing) or bronchospasm (the sudden contraction of smooth muscles in the lung, leading to the sensation of chest tightening). Both issues cause breathing difficulties that require urgent treatment.
If you take methotrexate, a cough can indicate a serious side effect called pneumonitis, inflammation of the lungs.
Environmental factors and infections
Our environment is also full of potential cough triggers. Environmental triggers include allergens, smoke, and pollution. Here are a few to consider.
- Allergens (e.g. pollen, dust, mold)
- Wildfire smoke
- Dry air
- Air pollution
The items in the above list might seem obvious, but other types of cough-triggering factors can be stealthy, including certain lung infections such as histoplasmosis or nontuberculous mycobacterial infection, which can mimic environmental causes and should be considered if symptoms persist. (Not-so-fun fact, my dear mom has had both of these at different times.)
- Histoplasmosis is a lung infection brought on by breathing in the Histoplasma fungus that’s common in certain areas, particularly around the Ohio and Mississippi Valleys in the United States.
- Nontuberculous mycobacterial infection occurs from a genus of bacteria that live in water and soil.
Not everyone who is exposed to these microbes will develop these infections, but they are worth considering, especially if you and your clinician rule out other obvious potential causes of cough. In my mom’s case in both instances, some tests confirmed the presence of these microbes, and treatment brought on relief. (Bringing me emotional relief too, I might add.)
Stress or habitual coughing
In rare cases, people can develop what’s called somatic cough syndrome, previously called psychogenic cough, where they have a cough without an obvious medical reason or trigger. This is a diagnosis of exclusion made only after medical causes are ruled out. Stress, anxiety, or obsessive-compulsive disorder (OCD) may contribute, but a diagnosis like this should only be made carefully by an experienced provider, to ensure they’re not dismissing your symptoms prematurely.
This topic needs to come with a disclaimer though, as I can attest that nothing can be more frustrating when it comes to healthcare than having someone tell you a symptom is “all in your head.” A good doctor will investigate all other potential cough causes before suggesting you have this syndrome. And they should not just send you on your way, but rather help you resolve the situation, which may mean referring you to a provider who specializes in mental health care and this unusual issue.
Dry cough causes vs. productive cough causes
You might have heard of coughs being described as either dry or productive. Unfortunately, “productive” in this case does not mean that the cough is slaying your to-do list of daily chores, work tasks, homework, etc. (If only!)
- Dry cough: “A dry cough is often a symptom of a cough without actually producing a mucus or sputum or secretions,” says Regina Pillai, MD, a board-certified pulmonologist with CLS Health.
- Productive cough: “A productive cough is often defined as you do have secretions along with the cough,” she says. Secretions can include mucus or blood and be clear, pus-like, or even yellow or green. This type of cough is also called a “wet” cough.
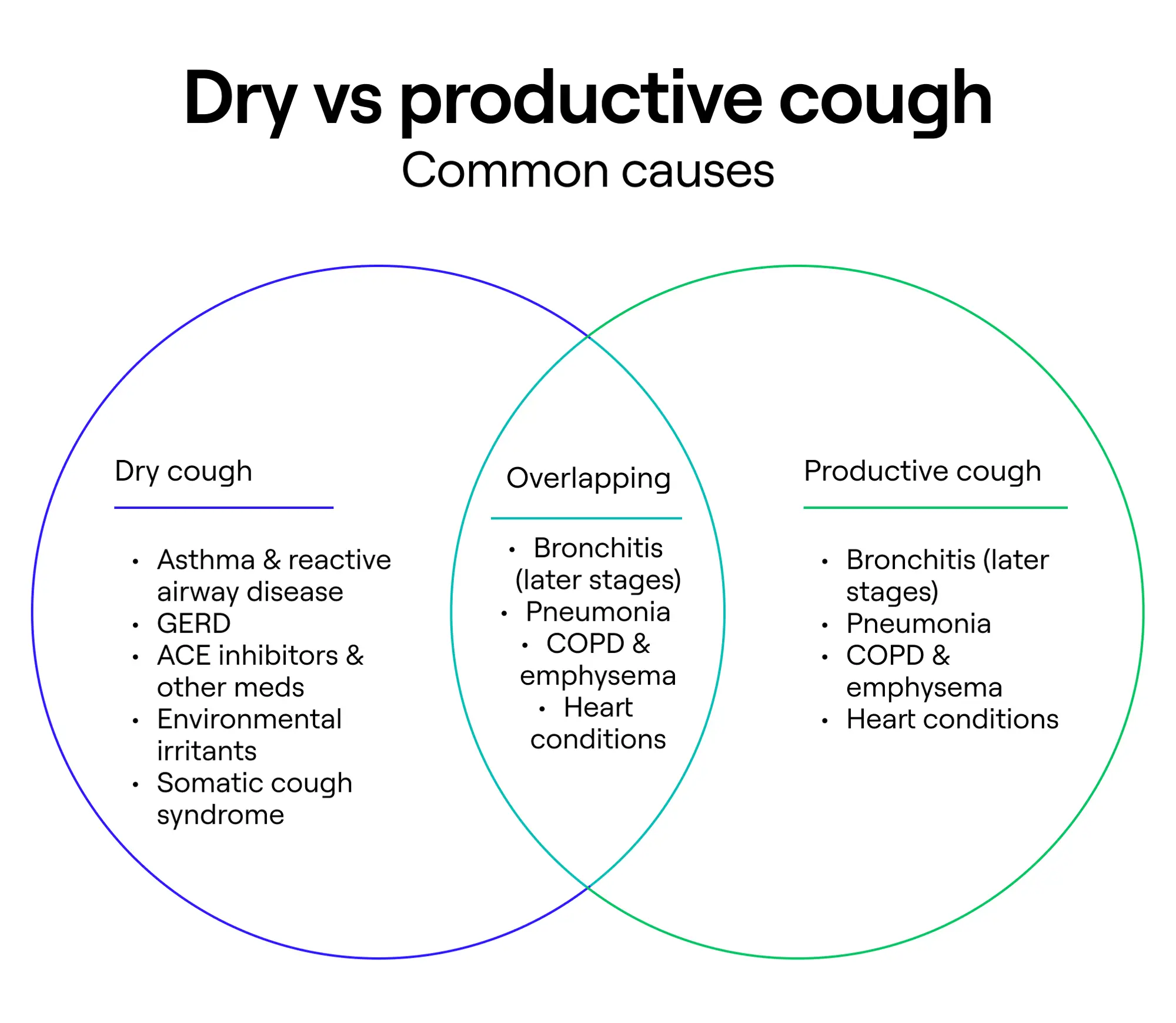
Dry vs. productive cough
When should I see a doctor for a cough that won’t go away?
Now that you know about common cough causes when you don’t feel sick, you might be wondering when you should get thee to a doctor or talk to a provider via telehealth options.
“A cough that's been present for more than eight weeks is a reason to see a physician,” says Dr. Pillai. Of course, if the cough is bothersome (aren’t they all?), you can talk to a doctor at any time; you don’t have to wait.
Some symptoms are red flags that you should see doctor asap:
- Fever or chills
- Unexplained weight loss
- Coughing up blood
- Shortness of breath
“Smokers with a cough that has gotten worse, see a doctor right then, because there could be other reasons for the cough that really need to be investigated,” Dr. Pillai says. “Any wheezing, any sense that you're getting more and more short of breath progressively, that is also an alarming sign to see a physician.”
General Medicine patient testimonial
What to expect at a doctor’s visit for chronic cough
When you talk to a doctor or other medical provider for a chronic cough, you can likely expect that they will ask you about your symptoms and your medical history.
If you’re in person, they may also examine you, including listening to your heart and lungs with a stethoscope and looking in your mouth, nostrils, and ears.
If your doctor suspects an infection or another illness, they may do some tests. Here are some that might come up.
- Blood tests: “Bloodwork like a CBC, a complete blood count, is always reasonable to look for infection and [look] at any other components of WBC count,” Dr. Pillai says. A WBC stands for white blood cell count and is useful for checking whether you have a specific type of airway disease called eosinophilic asthma, allergies, or another issue.
- Sputum culture: “If you’re producing sputum, it’s also reasonable to do a sputum culture if it's persistent,” Dr. Pillai says. Basically, you’ll provide the lab with a phlegm sample so they can check it for signs of infection.
- Nasal swab: If your doctor suspects an infection, they may swab your nasal (or throat) passages to test your secretions.
- Pulmonary function tests: These tests measure how much air you can inhale and exhale and how effectively you do so. (I have to undergo these regularly to assess the state of my eosinophilic asthma, and my pro tip is to ask for the gamified version they use for kids. I’ll never grow up.)
- Imaging: Your provider might recommend a chest X-ray or CT scan to view your long tissue and look for anything that could be contributing to your cough.
- Biopsy: In some cases, if nodules or masses are detected on imaging, you may need a lung biopsy, which is a procedure that takes a small sample of lung tissue to test it.
Self-care tips to manage and stop persistent coughing
Your provider can recommend the best self-care tips for managing your cough based on the reason for your cough. The ways to manage an asthmatic cough will be different from managing a cough resulting from, say, GERD or air pollution.
Sure, you might be tempted to reach for an over-the-counter cough suppressant, but if asthma or COPD is to blame, you should avoid these. That’s just one example why figuring out the underlying cause is so important, rather than managing a cough on your own with blanket recommendations. But a heart condition is another. If the cough is the result of fluid buildup in the lungs, for example, you’ll urgently need prescription medications to help counteract the issue and prevent breathing difficulties.
Consider your healthcare provider to be a detective who can help you solve the case and find solutions.
However, if you think the cough is from postnasal drip, you can certainly give an over-the-counter antihistamine or corticosteroid nasal spray a try, unless you have a reason to avoid these medications. A saline nasal rinse can also be a helpful solution.
If GERD is a prime suspect, avoiding trigger foods (such as spicy or tomato-based dishes) may ease your symptoms. You can also try taking an over-the-counter proton-pump inhibitor to help block stomach acid production in the short term until you can get checked out by a provider.
“I was prescribed antibiotics and an inhaler within minutes of my appointment. There is no greater way than to honestly say General Medicine saved my life. I am forever thankful.” —Helen, Virginia
Key takeaways
- So you have a cough that won’t go away, but you’re not sick? What should you do? Seeing a healthcare provider in these instances is always a good idea.
- A provider can evaluate you for underlying conditions, infections, or sensitivity to environmental triggers.
- The best way to treat a persistent cough will depend on the underlying cause.
- Need to see a doctor sooner rather than later? Schedule an appointment with a General Medicine provider.
General Medicine follows a strict editorial process, including using real experts to write our articles, vetted primary sources, fact-checking, a secondary medical review, and updates as necessary. This article was medically reviewed and fact checked by Ecler Ercole Jaqua, MD and Swapna Ghanta, MD.
FAQ
How to fix a never-ending cough?
If you have a never-ending cough, you may have an underlying condition, such as asthma, GERD, COPD, heart disease, or something else that’s causing it. Sometimes a cough can signal the start of an infection or can persist for some time after an infection has resolved. Additionally, changes in the environment, such as dry air, wildfire smoke, and pollution can drive a persistent cough. The best way to treat a cough will depend on what’s causing your cough. That’s why talking to a healthcare provider is always a good idea.
What is a heart failure cough?
A persistent cough can be a symptom of congestive heart failure, which means the heart is having trouble pumping blood to the rest of the body effectively. This can cause a cough because of fluid buildup in the lungs, which causes irritation.
What could a persistent cough be a symptom of?
A persistent cough might be a symptom that you’re recovering from an infection or that you have an underlying condition, such as asthma, COPD, heart disease, GERD, etc. However, keep in mind that environmental factors can also trigger a cough. These include air pollution, allergens, or dryer-than-usual air.
How do I know if my coughing is serious?
Many instances of ongoing coughing are not serious, since several things can irritate your airways. However, your cough might have a serious underlying cause, but the only way to find out is to get evaluated by a healthcare professional.
Why is my cough not going away after antibiotics?
Antibiotics kill bacteria, but not all coughs are caused by bacteria. Many coughs brought on by an infection are viral, and antibiotics cannot treat a viral infection. Other cough causes include underlying conditions, such as GERD, asthma, allergies, COPD, and more. Or an environmental trigger, such as wildfire smoke or car exhaust, could be to blame.
Our editorial standards
At General Medicine, we cut through the clutter to make health care clearer, faster, and easier to navigate. Every article is grounded in evidence-based research and peer-reviewed journals, reviewed by medical professionals, and written in accessible language that helps you make health decisions with confidence. We’re committed to ensuring the quality and trustworthiness of our content and editorial process by providing information that is up-to-date, accurate, and actually useful. For more details on our editorial process, see here.



