Jul. 22, 2025
Tonsillitis vs Strep Throat: Find Out What You Have in Minutes (and Treat It)

Jump to
Book a visit
$25 typical copay
$100 without insurance
Get expert care for your pain today.
That sore, scratchy throat that won't quit? It might be tonsillitis or strep—and figuring out which is key to feeling better fast.
Plenty of us have been there—googling tonsillitis vs strep throat at midnight with a flashlight under the covers, throat on fire, wondering if we really need to drag ourselves to urgent care. A sore throat is the pits, but not knowing what's behind it—or how to treat it—can make you feel even worse. Do you need antibiotics? Will it go away on its own? Should you just power through with tea and lozenges?
Here’s where it gets confusing: Tonsillitis and strep throat often look and feel almost identical—think sore throat, fever, and red, swollen tonsils. But they’re not the same thing. Tonsillitis is a general term that just means your tonsils are inflamed, and it’s often caused by a virus (which won’t respond to antibiotics), says Adam Carewe, MD. Strep throat, on the other hand, is caused by streptococcus bacteria and does require antibiotics to prevent complications. So while they can look and feel alike, how you treat them can be totally different.
From tonsillitis, streptococcus, strep throat, and beyond, this guide breaks down the symptoms, causes, and treatments so you can figure out what’s going on—and feel better fast. Whether you're trying to skip the waiting room or just want clarity, we’ve got you covered.
Understanding the difference between tonsillitis and strep throat
Knowing the difference between tonsillitis and strep is the first step to getting the right treatment—and feeling like yourself again.
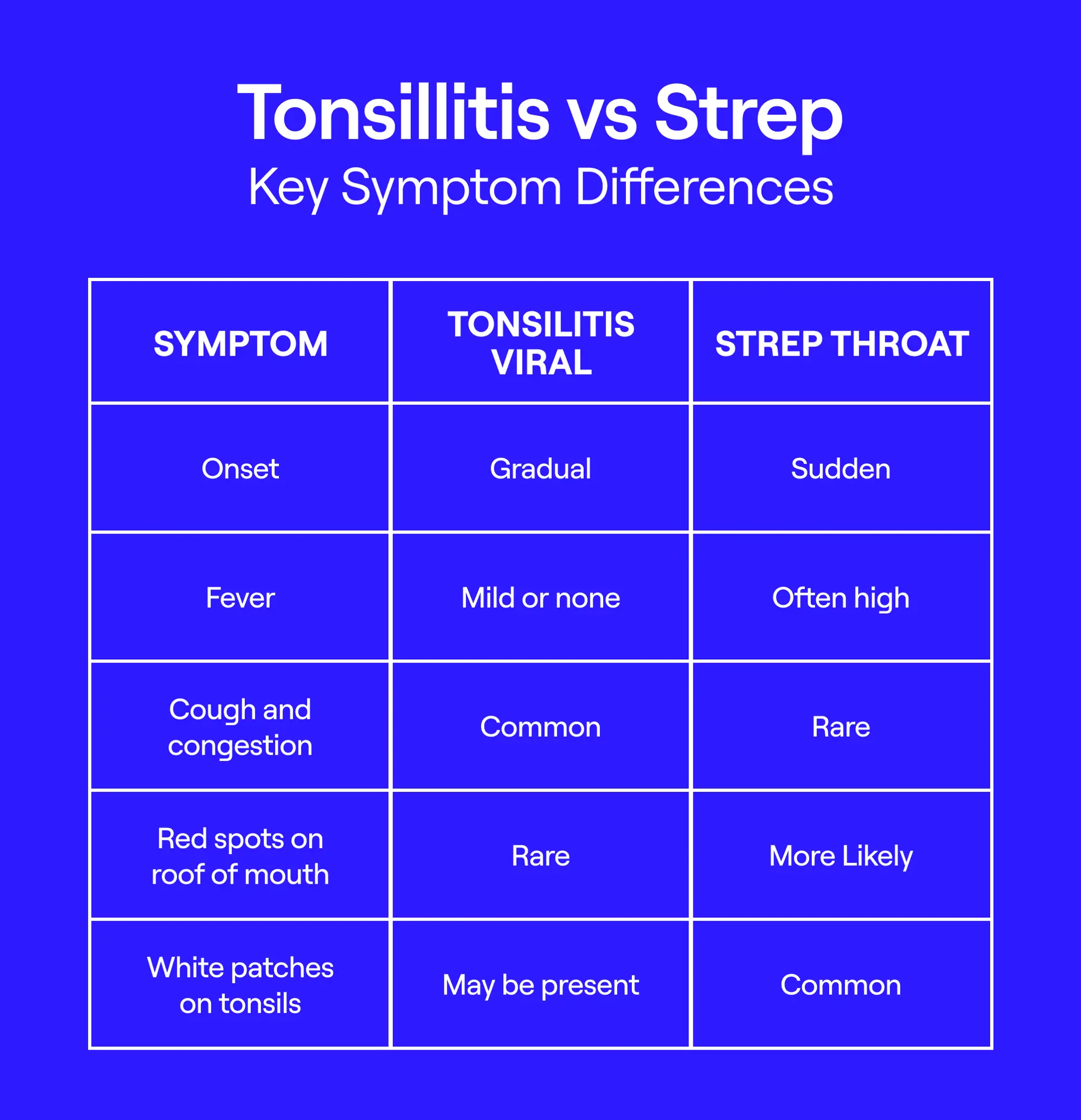
Tonsilitis vs. Strep: Key Symptom Differences
Tonsilitis
Tonsils are those two clumps of tissue at the back of your throat that act like bodyguards, helping filter out germs before they make you sick. But sometimes, they get overwhelmed—and infected—resulting in tonsillitis, or inflammation of the tonsils.
Tonsillitis is common, especially in kids, and it accounts for about 1.3% of all outpatient visits. Most of the time, it’s caused by viruses—the same ones responsible for the common cold (like rhinovirus, RSV, adenovirus, or even coronaviruses). When that’s the case, symptoms can usually be treated at home with rest, fluids, and comfort care—no antibiotics needed.
Strep throat
Strep throat, on the other hand, is caused by a specific type of bacteria: Group A Streptococcus. It's contagious and more serious than your average sore throat—but it’s less common. Only about 3 in 10 kids and 1 in 10 adults with sore throats actually have strep.
Here’s where it gets tricky: Strep throat can also cause tonsillitis. When the strep bacteria infect the tonsils, it leads to inflamed, swollen tonsils—just like in viral tonsillitis—but in this case, antibiotics are needed to treat the infection and prevent complications.
"All strep throat is tonsillitis, but not all tonsillitis is strep," Dr. Carewe says. "A quick test at the doctor’s office (strep test) is the only way to tell for sure."
Common symptoms: tonsillitis vs. strep throat
Strep throat vs tonsillitis? Sometimes it’s tough to tell. Tonsillitis and strep throat can feel almost identical at first—sore throat, swollen tonsils, and general misery—but there are some subtle differences that can help you (or your doctor) figure out what’s really going on. Here’s how to spot the key signs.
Tonsilitis symptoms
Tonsillitis can make your throat feel raw and sore—like a nasty cold or flu that just won’t quit. The tonsils usually look red, swollen, and irritated.
Other common tonsillitis symptoms include:
- Sore throat
- Trouble swallowing
- Fever
- Cough, congestion, or runny nose
- Headache
- Nausea or vomiting
- Earache
- Feeling worn out
Strep throat symptoms
Strep throat usually shows up suddenly and makes swallowing feel like sandpaper. Caused by bacteria (Group A strep), it’s more serious than viral tonsillitis and needs antibiotics.
Common strep throat symptoms:
- Sudden sore throat
- Pain when swallowing
- Fever
- Red, swollen tonsils
- White streaks or pus on the tonsils
- Swollen lymph nodes in the front of the neck
- Tiny red spots on the roof of the mouth (called petechiae)
Less common symptoms:
- Headache
- Belly pain
- Nausea or vomiting
- Scarlet fever-like rash
Pro Tip: If you’ve got a sore throat plus a cough, runny nose, hoarseness, or other symptoms like pink eye, it’s probably a virus—not strep, Dr. Carewe says.
Tonsil stones vs. strep throat: clearing up confusion
As if sore throats weren’t confusing enough, toss in tonsil stones and things get even murkier. "Tonsil stones are little white lumps that form in the tonsils when food, mucus, and bacteria get trapped," explains Dr. Carewe. They can look suspiciously similar to the white patches seen with strep throat—but the symptoms are usually way milder.
When it comes to tonsil stones vs strep, the key difference is in how you feel. Tonsil stones don’t typically cause fever or intense throat pain. Instead, they might give you funky-smelling breath or make your throat feel a little weird—like there’s something stuck back there. "If you feel mostly fine but notice white spots and bad breath, it’s more likely tonsil stones than strep," says Dr. Carewe. They’re harmless, often go away on their own, and you might even swallow them without realizing.
Still stumped? Don’t guess. "A doctor can help tell the difference," Dr. Carewe says. When in doubt, it’s always worth getting checked.
Tonsil stones quote from Adam Carewe, MD
How are tonsillitis and strep throat diagnosed quickly?
Tonsillitis and strep throat can look—and feel—pretty similar, but telling the difference matters. Why? Because only bacterial infections like strep need antibiotics. Viral ones? Not so much. Getting the right diagnosis helps avoid unnecessary meds (and side effects).
If you have obvious viral symptoms—like a cough, runny nose, or pink eye—your provider might not need to run any tests. A quick physical exam is often enough to confirm viral tonsillitis. But if those signs are missing, your doctor will likely do a test to be sure.
Here are the two main ways they figure out whether you’re dealing with strep vs. tonsilitis:
- Rapid antigen detection test (RADT): This is the quick one. A simple throat swab at your doctor’s office gives results in about 10–15 minutes. It checks for proteins from strep bacteria. If it’s positive, you’ve got strep. But if it’s negative, don’t rule it out just yet—false negatives can happen, so a backup test might be needed.
- Throat culture: This is the gold standard. It’s more accurate than the rapid test but takes longer—usually 1–2 days—because the sample has to be sent to a lab. Still, it’s the most reliable way to confirm or rule out strep.
Bottom line: Testing is key to getting the right treatment. Viral infections usually just need rest, fluids, and time. But if it’s strep, antibiotics are a must—not just to help you feel better faster, but to prevent it from spreading or leading to more serious complications.
A medical professional like those you can access virtually at General Medicine can help assess what’s going on, rule out anything serious, and guide you toward the right treatment that resolves your sore throat as soon as possible.
When to Test, When to Wait It Out
You might not need a strep test if:
- You have classic viral symptoms like a cough, runny nose, hoarseness, or pink eye
- Your sore throat is mild and improving with rest and fluids
- You’ve had similar viral infections before and know the drill
You should get tested if:
- Your sore throat comes on suddenly and is severe
- You have a fever of 101°F (38.3°C) or higher
- There’s no cough, but you notice swollen tonsils with white patches
- Your neck glands feel swollen or tender
- You’re unsure what’s causing your symptoms and want peace of mind
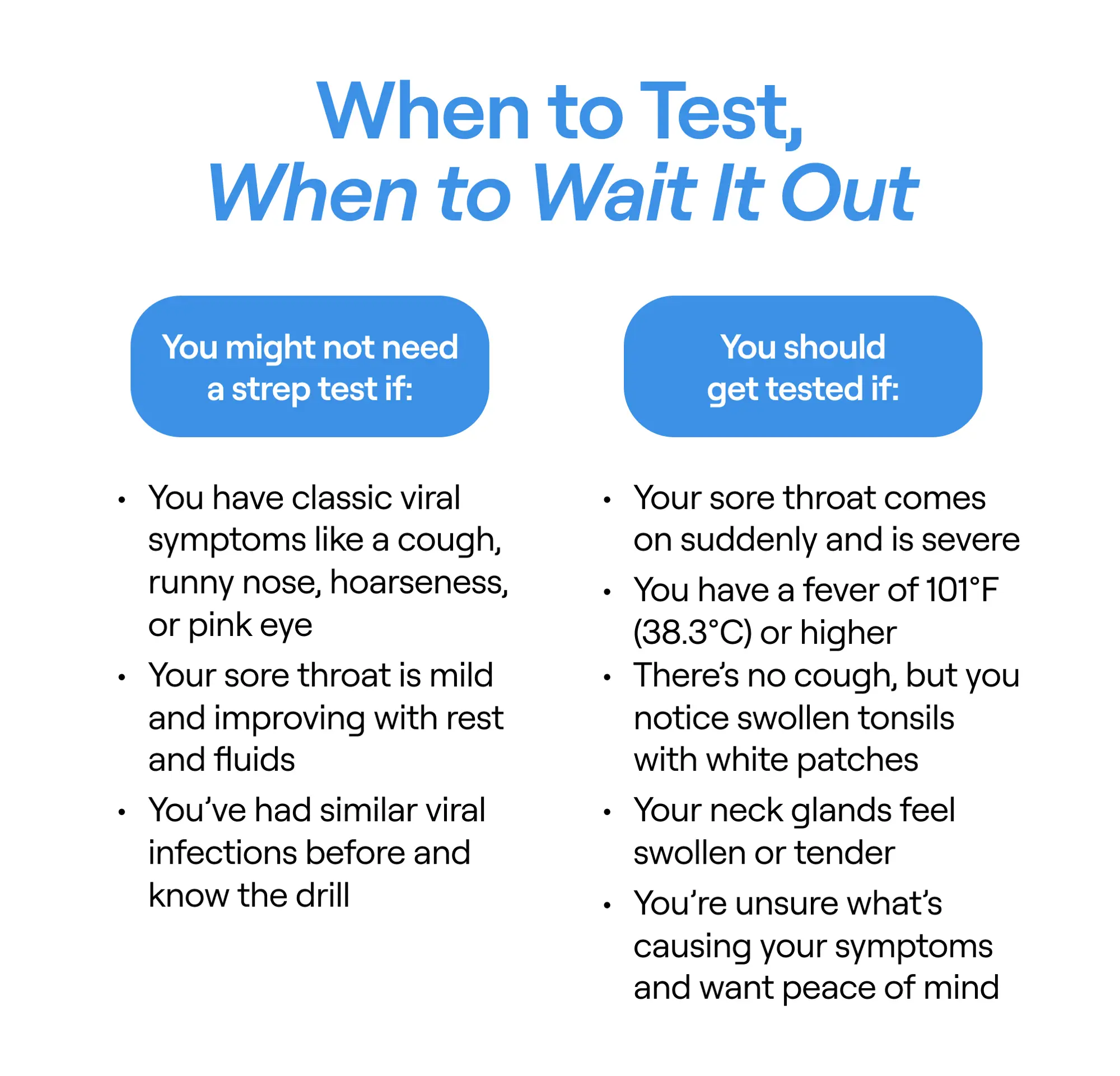
When to test for strep and when to wait
Risk factors for throat infections
Anyone can get a sore throat—but some people are more likely to catch one than others. Here are the top factors that can raise your risk:
- Kids get it more: Children, especially those between 5 and 15 years old, are prime targets for throat infections like strep.
- Cold weather season: Throat infections spike in the winter and early spring—when people are stuck indoors and germs spread more easily.
- Close quarters: Crowded places like schools, daycares, or offices make it easy for viruses and bacteria to jump from person to person. Sharing drinks or being near someone who's sick? Big risk.
- Poor hand hygiene: Not washing your hands regularly can lead to all kinds of infections—including those that mess with your throat.
- Weakened immune system: If you have a chronic condition like HIV or diabetes, or you're undergoing treatments like chemo, your body’s defenses are down—and infections can sneak in more easily.
- Other health issues: Conditions like seasonal allergies, sinus infections, or acid reflux (GERD) can irritate the throat and make you more vulnerable.
- Certain medications: Drugs that suppress the immune system (like immunosuppressants) can make it harder for your body to fight off throat infections.
- Irritants in the air: Smoke (even secondhand), pollution, and chemical fumes can inflame the throat and lower your resistance.
- Smoking: Whether you’re lighting up or just breathing it in, tobacco smoke irritates the throat and ups your risk of infection.
Treatment options for tonsillitis and strep throat
When it comes to treating a sore throat, the right approach depends on the cause—whether it’s viral tonsillitis or a bacterial infection like strep throat.
Tonsillitis treatment
Most cases of viral tonsillitis clear up on their own in a few days. The key? Let your body rest and focus on soothing the symptoms while your immune system does its thing.
Quick Relief Tips:
- Get plenty of rest (your body needs the downtime).
- Sip on cool drinks to calm the throat.
- Take acetaminophen (Tylenol) or ibuprofen to ease pain and bring down a fever. (Never give aspirin to kids under 16. It may lead to Reye syndrome in children.)
- Gargle with warm salty water (for older kids and adults).
- Suck on ice chips or popsicles.
- Use a clean humidifier or cool-mist vaporizer to keep the air moist.
- Drink warm tea with honey (for kids over 1) and stay hydrated with other bland, warm fluids like broth.
- Try throat lozenges with a mild anesthetic like benzocaine (not safe for young kids due to a possible choking risk).
- Spritz with an antiseptic throat spray (though studies say results may vary).
While these won’t cure tonsillitis, they can make things more bearable as you recover.
Strep throat treatment
Unlike viral tonsillitis, strep throat is bacterial—and that means antibiotics are essential.
- They help you feel better faster.
- They stop you from spreading strep to others.
- They prevent serious complications (like rheumatic fever) down the line.
What you’ll likely be prescribed:
- Penicillin or amoxicillin are the go-to options.
- If you're allergic to penicillin, no worries—there are safe alternatives.
While you wait for the antibiotics to kick in (usually 24–48 hours), use the same symptom-soothing tips as for tonsillitis: fluids, pain relief, and rest.
If your sore throat keeps making a comeback even after treatment, it could be chronic tonsillitis, says Dr. Carewe. In some cases, repeated infections may mean it’s time to talk to your doctor about removing your tonsils.
When to seek immediate medical attention
Most sore throats are more annoying than alarming—especially if they’re caused by a virus, which is usually the case. The good news? Viral sore throats typically clear up on their own in a few days with some TLC.
But if your sore throat isn’t going away—or it’s getting worse—it’s time to call in the pros.Certain symptoms can signal a more serious infection, like strep throat, or complications that may require antibiotics. Reach out to a healthcare provider if you or your child experience any of the following symptoms:
- Excessive drooling (especially in young kids)
- A fever of 101°F (38.3°C) or higher
- Pus or white patches at the back of the throat
- A red, sandpaper-like rash—especially in skin folds
- Trouble swallowing or breathing
- Swollen or tender lymph nodes in the neck
These red flags could point to a bacterial infection like strep or something more serious, such as rheumatic fever—both of which need medical treatment to avoid complications.
Complications of throat infections
Most throat infections clear up without much drama—especially when they’re treated properly. But in some cases, particularly with untreated strep, things can get a bit more serious. While complications are rare, they’re more likely to affect kids or people with weakened immune systems.
If strep bacteria spread beyond the throat, they can cause other infections, like:
- Painful abscesses (pockets of pus) around the tonsils or neck
- Ear infections
- Sinus infections
In even rarer cases, your body’s immune system can go a little haywire after the strep infection is gone. These complications aren’t caused by the bacteria directly—but by your immune system’s overreaction. They include:
- Rheumatic fever, which can affect your heart, joints, skin, and brain
- Post-streptococcal glomerulonephritis, a kidney condition that can cause swelling, dark urine, or high blood pressure
Getting an accurate diagnosis and timely treatment is essential—not just to feel better faster, but to avoid complications down the line. If your symptoms aren’t improving or seem to be getting worse, don’t wait to reach out to a healthcare provider.
Prevention tips for tonsillitis and strep throat
You can’t always dodge a sore throat—but a few smart habits can go a long way in keeping germs at bay. Since throat infections spread through respiratory droplets (think sneezes, coughs, or shared utensils), practicing good hygiene is your first line of defense.
Want to protect yourself and your family? Start here:
- Wash your hands regularly with soap and water—especially before eating or after being in public places.
- Don’t share food, drinks, or utensils with someone who’s sick.
- Cover your mouth and nose when you cough or sneeze—use a tissue or your elbow, not your hands.
- Toss used tissues right away (and wash your hands after!).
- If you or your kid has a fever or just feels crummy, stay home and rest until you’re back to normal. Avoid spreading the love (aka germs).
Good hygiene helps—but your immune system is your real MVP when it comes to fighting infections. Keep it strong with a few everyday wellness habits:
- Eat the rainbow. Load up on fruits and veggies to get the nutrients your immune system needs to thrive.
- Move your body. Regular exercise isn’t just good for your mood—it can help your immune system work better. In fact, one massive study found that adults who met fitness guidelines were about 50% less likely to die from flu or pneumonia.
- Sleep like it’s your job. Skimping on sleep messes with your immunity. Aim for 7–9 hours a night.
- Stay in your healthy weight range. Obesity is linked to weakened immune response.
- Ditch the smokes. Smoking makes it harder for your body to fight off infection.
- Drink less booze. Too much alcohol over time can chip away at your immune defenses.
Again, you might not be able to avoid every germ, but these simple steps can give your body the upper hand.
A sore throat can be a real pain—literally—but figuring out whether it’s tonsillitis or strep doesn’t have to be a guessing game. Because the symptoms can look so similar, getting an accurate diagnosis is crucial to making sure you get the right treatment (and avoid meds you don’t need).
If you're still not sure what's going on, a quick virtual visit with a medical provider through General Medicine can give you answers fast. They can check your symptoms, recommend convenient treatment options, and help you start feeling better—stat—all from the comfort of your home.
Key takeaways
- Tonsillitis is inflammation of the tonsils—and it can be caused by viruses or bacteria, including strep.
- Strep throat is a specific bacterial infection (from Group A Streptococcus) that often causes tonsillitis and requires antibiotics.
- Symptoms like sore throat, fever, and swollen tonsils overlap, but strep typically causes more severe pain and no cough.
- Tonsil stones can mimic strep visually, but they’re usually harmless and don’t come with fever or major discomfort.
- A quick strep test can help tell the difference, so you don’t take antibiotics unless they’re actually needed.
General Medicine follows a strict editorial process, including using real experts to write our articles, vetted primary sources, fact-checking, a secondary medical review, and updates as necessary. This article was medically reviewed and fact-checked by Pallabi Sanyal-Dey, MD and Marjory Bravard, MD.
FAQ
How do you tell the difference between tonsillitis and strep?
Tonsillitis and strep throat can feel super similar—both cause a sore throat, swollen tonsils, and general blah-ness—but there are a few clues that can help you tell them apart. Tonsillitis can be caused by either a virus or bacteria and often comes with cold-like symptoms like a runny nose or cough. Strep throat, on the other hand, is caused by a specific bacteria (group A strep) and usually hits harder and faster—with a really sore throat, fever, red and swollen tonsils (sometimes with white patches), and no cough. "You can’t tell by eye which germ is to blame, so a quick throat swab test is the only sure way" to know, says Poushali Bhattacharjee, MD.
Do you need antibiotics for tonsillitis?
It depends. If it’s viral tonsillitis, you can usually ride it out—most cases clear up on their own within a few days with rest and home remedies. But it’s caused by bacteria (like strep throat), that’s a different story. You need antibiotics to knock out bacterial infections. Without treatment, strep can spread or lead to serious complications like rheumatic fever or kidney problems—especially in kids, people with chronic health conditions, or anyone with a weaker immune system.
How to identify strep throat without tonsils?
Yep, even if you’ve had your tonsils removed, strep throat can still strike. That’s because strep "bacteria infect the throat tissue—not just the tonsils," explains Dr. Carewe.
Even without tonsils, your provider will still be on the lookout for common symptoms including a sudden, severe sore throat, fever, pain when swallowing, and tender "lumps" in the front of the neck (i.e., swollen lymph nodes), says Dr. Bhattacharjee.
Still not sure? You’ll need a strep test to know for certain, Dr. Carewe adds. The symptoms can look like other infections, so it’s best to get checked.
Does strep or tonsillitis go away on its own?
If it’s viral tonsillitis, the answer is yes—it usually goes away on its own in a few days with some rest and TLC. But strep throat? That’s a whole different ballgame. You’ll need antibiotics to treat it properly since it’s a bacterial infection. Left unchecked, strep can lead to serious complications like rheumatic fever or kidney issues. So if you suspect strep, don’t tough it out—get evaluated and treated.
Does strep A feel like tonsillitis?
Yep, strep A can definitely feel like tonsillitis—because technically, it is a type of tonsillitis caused by group A strep bacteria. The symptoms often overlap: sore throat, swollen tonsils, pain when swallowing, and maybe a fever. But strep tends to come on more suddenly and feels more intense. You might also notice red spots on the roof of your mouth, white patches on your tonsils, or swollen lymph nodes in your neck. The key difference? Strep is bacterial and needs antibiotics, while many cases of tonsillitis are viral and clear up on their own.
Our editorial standards
At General Medicine, we cut through the clutter to make health care clearer, faster, and easier to navigate. Every article is grounded in evidence-based research and peer-reviewed journals, reviewed by medical professionals, and written in accessible language that helps you make health decisions with confidence. We’re committed to ensuring the quality and trustworthiness of our content and editorial process by providing information that is up-to-date, accurate, and actually useful. For more details on our editorial process, see here.



