
Jump to
Book a visit
$25 typical copay
$100 without insurance
Get a legitimate doctor's note online today for work or school.
Pancre-what? Your pancreas sits behind your stomach, where it produces and secretes digestive enzymes, and also the hormone insulin. It might not be the first organ you think about when abdominal pain or other symptoms strike, but it could be the culprit, especially if you have pancreatitis or another pancreas problem.
Let’s pretend our internal organs are having a popularity contest. The heart is probably a fan favorite for most, just because of how we associate it with love. Plus, we can feel it beat. But what’s an organ that would totally get picked last, or forgotten entirely? The pancreas.
It’s one of those organs you might not think about at all—unless, that is, something goes wrong. And even then, when symptoms initially show up, you might not realize they could be related to your pancreas, an organ that hangs out behind your stomach and is involved in digestion and hormone secretion, especially insulin.
But the pancreas truly is a star, and if something goes wrong with it, seeking care early is crucial. I’ve got a personal tale. In my mid-20s, I suddenly had extreme abdominal pain with no explanation. It was so severe that I went to the ER, which kicked off a week-long stay in the hospital where I was served a host of intravenous (IV) cocktails—not exactly the vacation from work I was looking for. Could they have at least hung one of those tiny umbrellas on my IV?
After several tests, the doctors on the case determined I had gallstone pancreatitis. (More on this condition below). After some rest and supportive care, they finally sent me on my way. But ever since then, and after learning more about the pancreas, I’ve been intrigued by the organ. It does some nifty things in the body.
In this article, we’ll let the pancreas shine by highlighting some of its functions, red flags to watch for, symptoms of pancreatitis, and more.
What is pancreatitis?
Pancreatitis in simple terms is inflammation of the pancreas that causes swelling and pain that may spread to your back.
What is pancreatitis?
The top two causes are gallstones and heavy alcohol consumption. Limiting or avoiding alcohol—especially if you have other risk factors—can help lower your risk.
- Gallstone pancreatitis: Your biliary system includes your liver, gallbladder, and pancreas, and they share a common bile duct. Think of these organs as dorm rooms and the duct as a shared hallway. If a gallstone blocks the common bile duct, it prevents digestive enzymes from leaving your pancreas. Pressure builds and the activated enzymes start digesting your pancreas instead of breaking down food. Yikes!
- Heavy alcohol consumption pancreatitis: Researchers believe alcohol and its byproducts can put the pancreas at risk of damage from substances that do not normally cause pancreatic damage.
Other causes of pancreatitis include medication side effects, infections, autoimmune disease, genetics, and more. Pancreatitis can be acute (temporary) and chronic (ongoing).
- Acute:cute: A sudden inflammation of the pancreas that can range from mild and self-limiting to severe and life-threatening, depending on the cause and extent of inflammation.
- Chronic: This is a long-term progressive condition that can cause ongoing damage.
Not all pancreas problems involve pancreatitis, though. Other conditions that can affect the organ include diabetes and pancreatic cancer—but don’t panic.
7 common symptoms of pancreas problems
1. Abdominal pain
Upper abdominal pain that radiates to the back could signal pancreatitis. It may feel worse during movement, coughing, lying flat, or during or after eating. (For me, it felt like someone had stabbed me, not that I’ve ever been stabbed before. Just guessing.)
2. Nausea and vomiting
Persistent nausea or vomiting (or as my mom likes to call it “praying to the porcelain gods”) could be a sign of a digestive issue, including pancreatitis. Of course, these symptoms are common for many other conditions as well, including foodborne illness, gastroenteritis, viruses, and more.
3. Unintentional weight loss
Unintentional weight loss could be a sign of type 1 diabetes (see #6), chronic pancreatitis, pancreatic cancer, and pancreatic exocrine insufficiency, in which the pancreas doesn’t produce enough digestive enzymes, often as a result of chronic pancreatitis.
Depending on the underlying cause, the mechanisms might involve insufficient hormone production or release, poor absorption since the pancreas produces enzymes that help you digest certain nutrients, and pain leading to lack of appetite.
4. Oily, foul-smelling stools
This symptom, also called steatorrhea, suggests trouble with fat absorption from foods. Greasy or smelly poo results from fat ending up in stool. It could indicate pancreatic exocrine insufficiency, pancreatic cancer, a lack of bile acid, or diseases affecting the small intestine.
5. Bloating and digestive issues
Most people have experienced bloating or digestive issues at some point, or several, in their lives from something they ate, illness, their menstrual cycle, etc. But if bloating or digestive issues occur often or are ongoing, you should talk to a healthcare provider to get to the bottom of your symptoms.
Pancreatic cancer or acute or chronic pancreatitis are potential underlying causes. Pancreatitis can cause pancreatic pseudocysts, which are fluid-filled sacs of accumulated enzymes that can cause bloating and pain.
6. Elevated blood sugar and diabetes
Specialized cells in your pancreas secrete the hormone insulin, which signals your cells to uptake glucose as a source of energy from the foods you eat. When the pancreas doesn’t produce enough or any insulin or when cells stop responding as well to insulin’s signals (insulin resistance), then a person has a form of diabetes.
- Type 2: You have insulin resistance, and your pancreas may have stopped producing adequate insulin after an increased demand for the hormone has “worn out” your insulin-producing cells.
- Type 1: Your pancreas doesn’t make insulin, and you need to take insulin as a medication to treat this autoimmune disease that attacks pancreatic cells. It’s usually diagnosed in childhood.
- Latent autoimmune diabetes in adults (LADA), or Type 1.5: This autoimmune condition means your body mistakenly attacks the pancreas. You might still produce insulin, but you will likely eventually need insulin therapy. As the name suggests, LADA is typically diagnosed in adulthood, though, because of this, the condition is sometimes initially misdiagnosed as Type 2.
7. Jaundice (yellowing of skin and eyes)
When your body breaks down red blood cells, it produces a bilirubin, a yellow pigment. When this pigment accumulates in the body, rather than being processed in the liver and excreted through waste, you might develop yellow skin or yellow eyes.
If your biliary ducts are blocked, your liver can’t excrete bilirubin in bile. Blockages can occur from gallstones or pancreatic tumors.
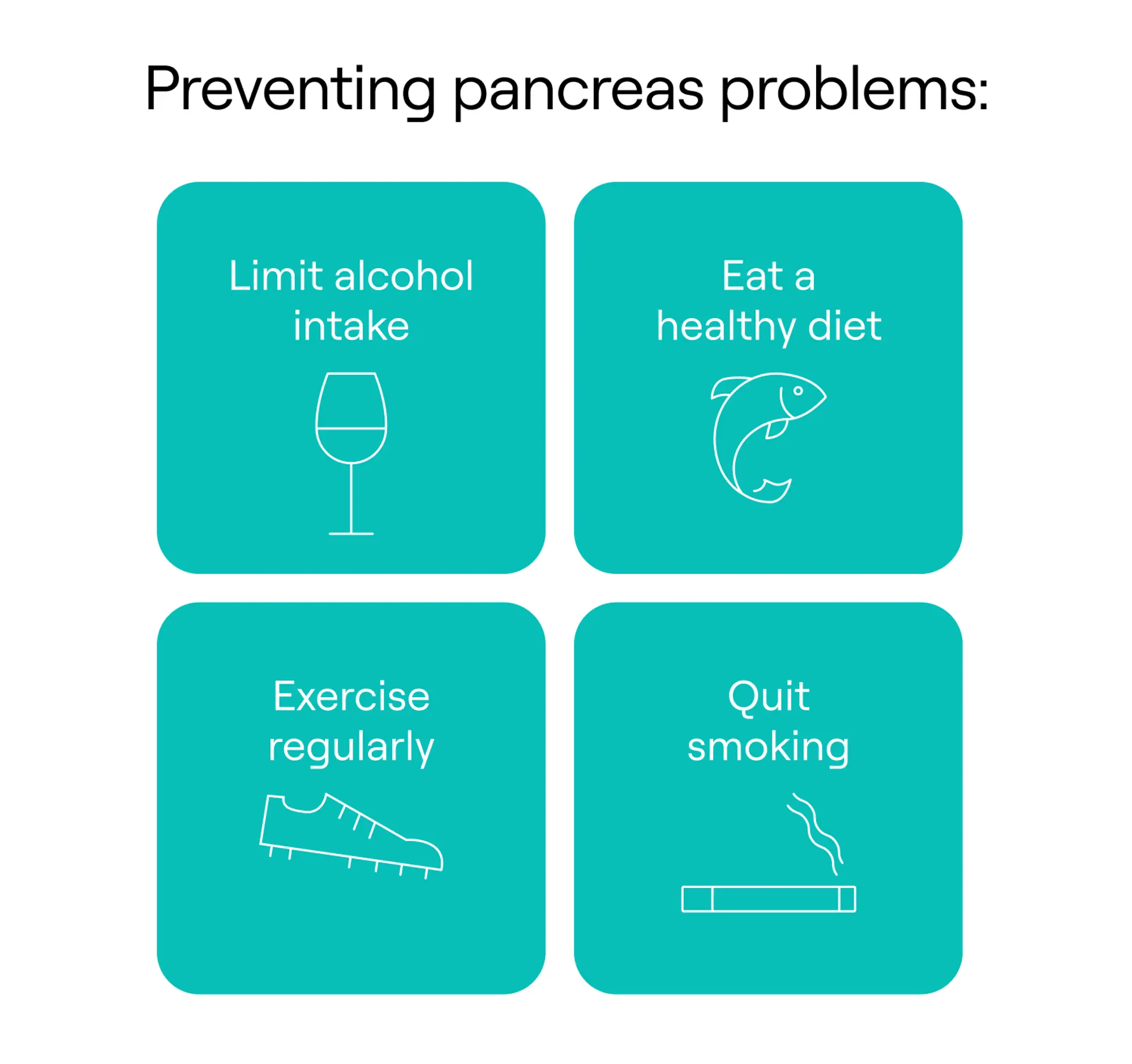
Preventing pancreas problems
When to seek immediate medical attention
You should seek immediate medical attention if you have severe or ongoing abdominal pain that’s accompanied by the following:
- Fever or chills
- Nausea or vomiting
- Blood in your stool or vomit
- Persistent digestive issues, such as diarrhea
- Jaundice
- Rapid heart rate
- Shortness of breath
- Unexplained weight loss or poor appetite
Seeking medical care involves the question: Is this an ER visit, an urgent care visit, a check-in with my regular doctor, or a telehealth matter? I wish the world had a flowchart for every scenario so we never had to guess. So my goal here is to offer you some guidance.
The above symptoms in combination with abdominal pain are reasons to seek urgent medical care, typically by going to an emergency room.
However, if you are experiencing unexplained minor abdominal pain, nausea, indigestion, or other gastrointestinal symptoms, and you can’t see your usual doctor, an urgent care clinic is a good choice.
If you’re already established with a primary care physician or nurse practitioner, you can schedule an appointment or reach out in your patient portal with your questions, especially if your usual clinic is relatively responsive.
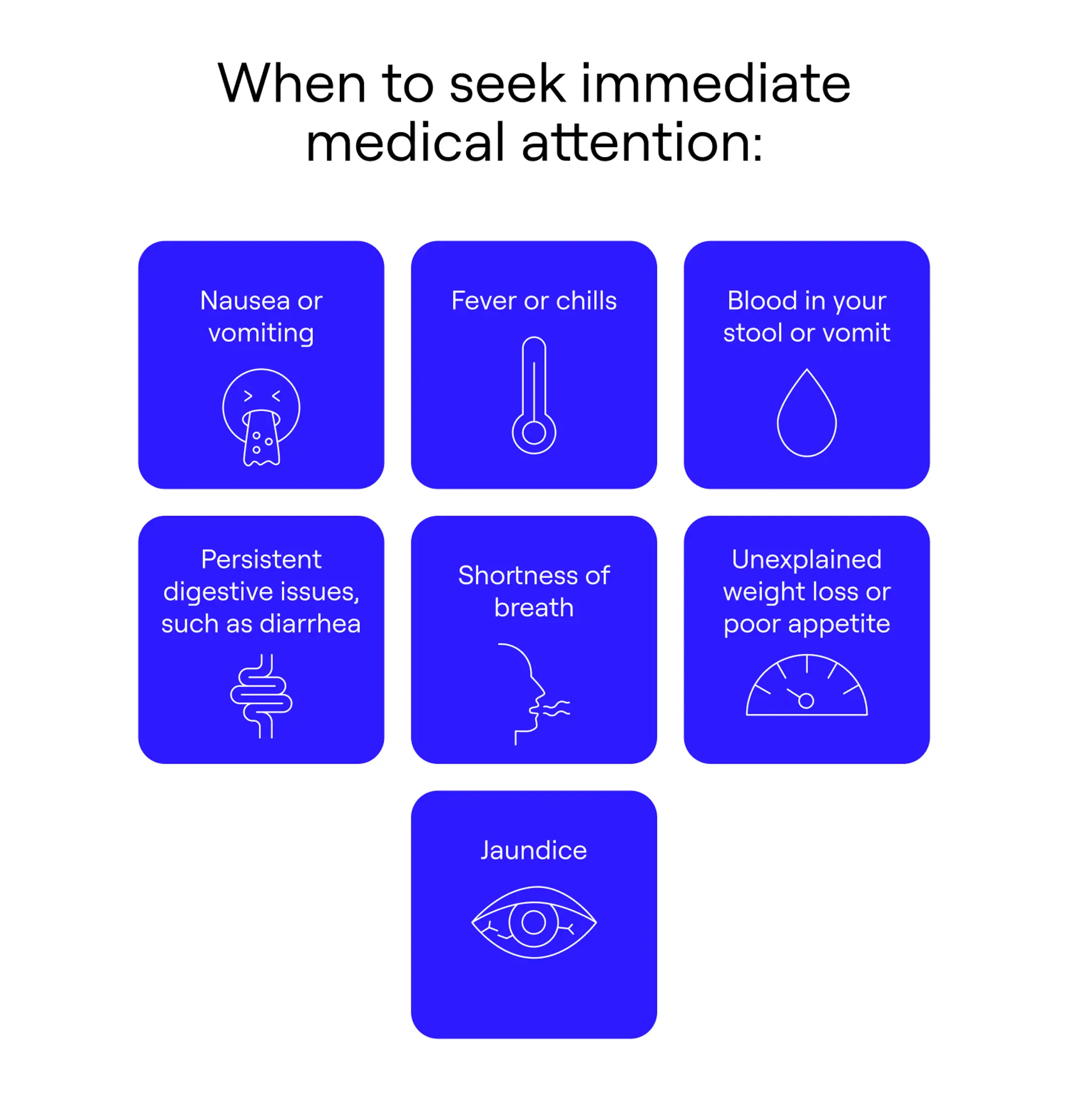
When to seek immediate medical attention
Another great option is to schedule a telehealth appointment. This can be especially helpful if you don’t have an established doctor or are pressed for time (aren’t we all?) or have an unpredictable schedule and can’t easily make an in-person appointment. (I’m over here raising my hand.)
During a telehealth visit, a care provider can walk you through any necessary next steps to take and answer your immediate questions. Telehealth providers can also offer you guidance on whether you need immediate in-person medical care based on your symptoms or if you can treat them at home. I’ve certainly used a telehealth option to help me decide what to do during various medical conundrums.
“General Medicine helped me get the imaging and blood work I needed, referred me to the right specialists, and even helped me find a new family doctor.” —Bridget, Mississippi.
Diagnosing pancreas problems
Your care team may use several diagnostic tools for determining if you have an issue with your pancreas, and if so, what the nature of it is.
- Medical history and symptomology: Your provider will likely ask you about your medical history, your immediate family’s medical history, and your current symptoms.
- Physical exam: If necessary, your provider will examine your abdomen. This might mean checking for distension, tenderness, and more.
- Biomarkers: Some biomarkers (blood, urine, or fecal analysis) can be helpful for checking pancreatic function. These may include: digestive enzyme levels, electrolyte levels, fasting insulin, glucose tests, antibodies, triglyceride levels, C-reactive protein, BUN, hematocrit, full blood count, and even DNA testing.
- Imaging: Several imaging tests can determine structural issues, such as gallstones, swelling, liver function, and more. These include: CT scan, MRI, ultrasound, and stool tests that can investigate enzymes and issues with fat absorption.
- Procedures: Some imaging techniques to view the digestive tract may involve undergoing sedation or general anesthesia. These include endoscopic ultrasound, which involves inserting a flexible tube down the throat, and endoscopic retrograde cholangiopancreatography ( ERCP), which uses endoscopy combined with an X-ray to view bile and pancreatic ducts.
- Medications: In some cases, pancreatitis is autoimmune. To diagnose this type, physicians sometimes prescribe a steroid trial (where you take corticosteroids) to see how you respond.
Pancreatitis treatment overview
If you suspect you have pancreatitis, you may be wondering how it’s treated. Seek medical attention—either from your trusted provider or a full-service care marketplace like General Medicine—so that your team can determine the best treatment option for your situation.
Treatment for acute pancreatitis often involves hospitalization, hydration, digestive rest, and pain management. (This was the case for yours truly.) If you have an infection, you will need an antibiotic. If you have gallstone pancreatitis, you may need surgery to remove the stone or even the whole gallbladder to prevent recurrence, though sometimes stones resolve on their own (as was the case for me).
Treatment for chronic pancreatitis might involve a mix of lifestyle changes (such as abstaining from alcohol), medical treatments or procedures, and more. Your provider might drain pseudocysts or recommend a pancreatoduodenectomy (Whipple procedure), which removes the pancreatic head, duodenum (first part of the small intestine), gallbladder, and bile duct. They may also prescribe digestive enzymes, pain-relief meds, and antioxidants, including multivitamins, selenium, and methionine. However, you should consult a provider first before taking these on your own.
Preventing pancreas problems
Lifestyle changes are not a failsafe guarantee that you won’t develop pancreas problems, but you can take steps to reduce your risk of an issue.
- Limit alcohol intake: Some public health authorities, including the WHO, advise that no amount of alcohol is safe, but recommendations vary by country. If you don’t drink, avoid starting. If you do drink, consider reducing your intake or eliminating alcohol altogether.
- Exercise regularly: Physical activity helps your body manage glucose and insulin more effectively, reducing your risk for Type 2 diabetes. Find activities you love, which can help you stick with the healthy habit.
- Quit smoking: Smoking is a risk factor for many cancers, including pancreatic. It’s also a risk factor for major health issues. If you smoke, talk to your doctor about a cessation method that’s right for you. You got this!
- Eat a healthy diet: Overconsumption of ultra-processed foods, refined carbohydrates, and sugar can contribute to the development of Type 2 diabetes. For those recovering from pancreatitis or with pancreatic enzyme insufficiency, avoiding high-fat foods such as fried items, fatty cuts of meat, and processed meats can reduce symptoms. Healthy fats from sources like fish, nuts, and olive oil can still be part of a balanced diet for most people. Other digestive irritants that your doctor may recommend avoiding, either temporarily or long term, include caffeine, spicy foods, and raw garlic or onions.
Key takeaways
- The pancreas is a remarkable organ responsible for producing and excreting digestive enzymes and the hormone insulin.
- Common issues with the pancreas include pancreatitis and the various forms of diabetes.
- A less common but major concern is pancreatic cancer.
- If you’re experiencing abdominal pain or digestive issues talk to a doctor asap to determine your next steps.
General Medicine follows a strict editorial process, including using real experts to write our articles, vetted primary sources, fact-checking, a secondary medical review, and updates as necessary. This article was medically reviewed and fact checked by Swapna Ghanta, MD, and Ecler Ercole Jaqua, MD.
FAQ
What are the first signs of a bad pancreas?
You might have pancreatitis or another issue with this crucial organ if you experience unexplained abdominal pain, nausea or vomiting, weight loss, oily or foul-smelling stools, bloating or other digestive issues, high blood sugar, or jaundice.
How do I get my pancreas back to normal?
How to get your pancreas back to normal will depend on the cause of any issues. If you’re experiencing unexplained symptoms that you suspect are related to your pancreas, seek medical treatment right away.
What are the symptoms of stage 1 pancreatic cancer?
Stage 1 pancreatic cancer is often asymptomatic. When symptoms do occur, they may include changes in bowel habits, mild abdominal discomfort, or, less commonly, jaundice, weight loss, or new-onset diabetes.
How to cleanse your pancreas?
You cannot “cleanse” your pancreas. However, healthy lifestyle changes, such as eating a healthy diet and limiting or abstaining from alcohol, can reduce your risk for pancreas problems.
Our editorial standards
At General Medicine, we cut through the clutter to make health care clearer, faster, and easier to navigate. Every article is grounded in evidence-based research and peer-reviewed journals, reviewed by medical professionals, and written in accessible language that helps you make health decisions with confidence. We’re committed to ensuring the quality and trustworthiness of our content and editorial process by providing information that is up-to-date, accurate, and actually useful. For more details on our editorial process, see here.



