Jump to
Book a visit
$25 typical copay
$100 without insurance
Get expert care for your pain today.
Wondering how to stop a burning sensation after urinating? From pesky UTIs to kidney stones (and even dehydration), figuring out the cause is the first step to real relief.
If you’ve ever frantically Googled “how to stop a burning sensation after urinating” while squirming on the toilet, you’re in good company. Dysuria (the medical term for burning when peeing) is surprisingly common—about 3% of adults over 40 are dealing with it at any given moment—making it the number-one urinary complaint doctors hear.
Still, a painful pee can come as a total shock—cue the uh oh, that can’t be good panic spiral. Your mind starts racing: UTI? Kidney stone? Did that new body wash betray me? In many cases, the answer is simple—a urinary tract infection (UTI), which is common and totally treatable. But if you’ve found yourself wondering “why does it burn when I pee?” and the sting won’t quit, it could be something else entirely. And here’s the thing: some causes can turn into bigger problems if ignored or treated the wrong way.
That’s why playing Dr. Google won’t do you any favors. Instead, let’s cut through the confusion. Ahead, we’ll break down the most common reasons your pee burns, how doctors figure out what’s really going on, and what you can do right now to find relief—and keep future bathroom trips pain-free.
What causes burning when you pee?
“Burning with urination is a symptom, not a diagnosis,” says Jerry Weinberg, MD, a urologist at Northern Westchester Hospital. “While it's most commonly associated with a urinary tract infection, it can be a sign of many other conditions.” Here, we break down the most common ones.
Burning with urination quote from Justin Houman, MD, FACS
- UTIs
- STIs
- Vaginitis
- Cystitis
- Prostate problems
Urinary tract infection (UTI) in women and men
If your pee feels like fire, chances are good it’s a UTI. These are among the most common bacterial infections out there—affecting millions each year—and those assigned female at birth get them more often than those assigned male.
A UTI happens when bacteria (usually E. coli) sneak into the urethra (the tube that carries urine out of your body) and make their way to the bladder. They can also affect the ureters (the tubes that carry urine from the kidneys to the bladder) or kidneys.
The result? Burning pee happens because the inflamed urethra or bladder lining is irritated by urine. This can be related to urine becoming more acidic or more alkaline due to overgrowth of bad bacteria. All of this may manifest as a constant urge to go, and that “didn’t I just pee?” feeling. Left untreated, a UTI can spread to your kidneys and cause serious complications, so don’t wait to get checked.
Sexually transmitted infections (STIs)
Nothing kills the mood faster than painful urination after sex—and some sexually transmitted infections (STIs) are to blame.
Chlamydia, gonorrhea, trichomoniasis, and genital herpes can all make peeing hurt. The pain itself is typically from lesions caused by these infections making contact with urine—not by a urethral infection itself. Other red flags: itchiness, unusual vaginal discharge, and in the case of herpes, blisters or sores around your genitals or rectum.
And while the stigma is heavy, STIs are extremely common. In fact, in 2023 alone, more than 2.4 million cases of chlamydia, gonorrhea, and syphilis were reported in the U.S. So if burning pee turns out to be from an STI, know you’re far from alone—and treatment is available.
Vaginitis
For people assigned female at birth, sometimes the burn comes from vaginal inflammation, aka vaginitis. This condition has several causes:
- Bacterial vaginosis: an overgrowth of bacteria that throws off your vagina’s balance.
- Yeast infections: usually caused by Candida albicans.
- Trichomoniasis: a sexually transmitted infection caused by a parasite.
- Atrophic vaginitis (aka genitourinary syndrome of menopause): thinning of the vaginal lining after menopause or ovary removal, which can cause dryness, burning, and irritation.
Along with painful urination, watch for other clues: discharge that looks or smells different, itching or irritation, pain during sex, or light spotting.
Prostate problems
For people assigned male at birth, the prostate—normally walnut-sized and sitting just below the bladder—can be the source of serious pee problems.
When the prostate acts up, urination can get uncomfortable. Two common culprits are:
- Prostatitis: inflammation of the prostate (sometimes caused by infection), which can cause burning, difficulty peeing, and pain in the groin, pelvis, or genitals.
- Benign prostatic hyperplasia (BPH): an enlarged prostate, common in people over 50. As it grows, it squeezes the urethra, slowing or blocking urine flow. Over time, the bladder muscle can weaken, making peeing even trickier—and yes, more uncomfortable.
Kidney stones
If peeing burns and your back feels like it’s staging a protest, kidney stones might be to blame. These rock-like clumps form when certain chemicals in your urine—like calcium, oxalate, or uric acid—decide to clump together instead of flushing out smoothly. About 1 in 10 people will get a kidney stone in their lifetime, so they’re more common than you might think.
Normally, your kidneys filter waste and excess minerals from your blood, sending them out through urine. But when there’s too much of certain chemicals and not enough water to dilute them, crystals can form and harden into stones. Tiny stones may sneak out of the body without much fuss, but larger ones often get stuck in the ureter (the tube connecting kidney to bladder). That’s when things get painful—sometimes very painful. Think: trying to pass a jagged pebble through a straw.
And kidney stones don’t just cause burning pee. They can come with a grab bag of other symptoms, including:
- A sudden, intense urge to pee
- Frequent urination
- Dark or bloody urine (sometimes only visible under a microscope)
- Nausea or vomiting
- Sharp, cramping pain in the back or side
- Pain at the tip of the penis (for people with penises)
Sometimes, if a stone blocks the flow of urine completely, it can even cause kidney damage. That’s why it’s always a smart idea to check in with your provider, especially if you have other symptoms.
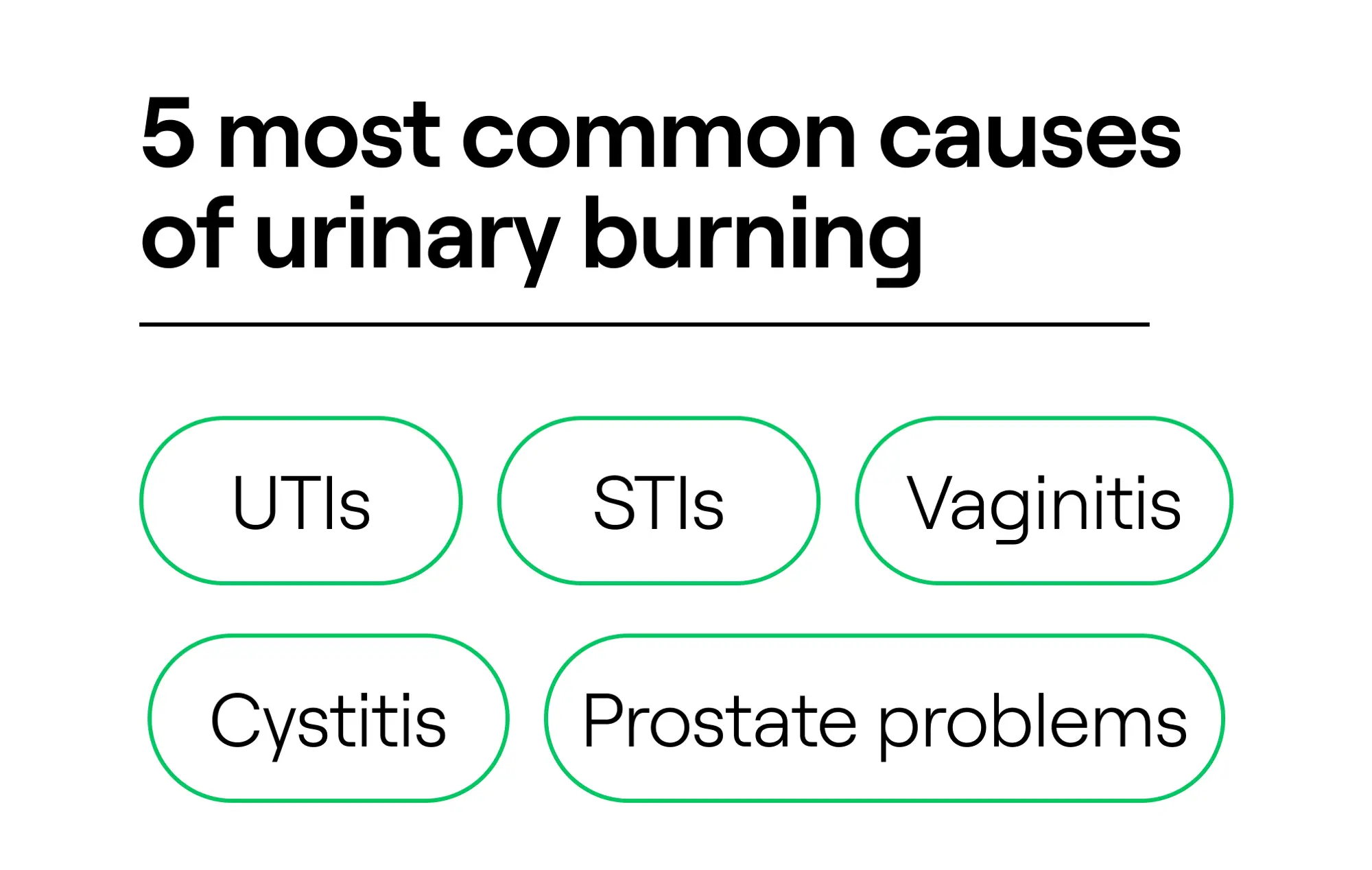
Most common causes of urinary burning
Cystitis
If every trip to the bathroom feels like fire, you might be dealing with an inflamed bladder (known as cystitis). It has a few different triggers, from a straightforward bacterial infection (the most common cause) to chemical irritants, pelvic radiation or chemo, or a chronic condition called interstitial cystitis (aka bladder pain syndrome).
Burning pee is the headliner symptom, but cystitis can bring a whole supporting cast:
- A nonstop urge to pee (even if little comes out)
- Peeing tiny amounts, way too often
- Blood in your urine (sometimes making it pink or red)
- Cloudy or funky-smelling urine
- Pressure or discomfort in your pelvis or lower belly
- Low-grade fever
Think you might have a bladder infection? Don’t wait it out. Untreated cystitis can climb up to your kidneys, where it can cause more serious—and sometimes permanent—damage. A quick trip to your provider can save you from bigger trouble later.
Irritants
Love your lavender bubble bath? Your private parts may not. Personal care products loaded with fragrances or harsh chemicals can irritate delicate urethral tissue, leading to painful urination, says Justin Houman, MD, FACS, of Tower Urology at Cedars-Sinai Medical Center.
Common culprits include:
- Vaginal sprays and douches
- Perfumed soaps or bubble baths
- Scented laundry detergents or toilet paper
- Spermicides and even some tampons
Sometimes the result is noninfectious vaginitis—basically irritation or inflammation of the vulva and vagina without infection. Remember: vaginitis is infamous for making pee feel fiery.
So if your burning pee lines up with a new product, ditch the culprit and see if things improve.
Dehydration
Here’s a less obvious cause of pain when peeing: you’re just not drinking enough water.
When you’re dehydrated, urine becomes more concentrated, which means higher levels of salts, minerals, and waste products—all of which “can irritate your bladder lining and urethra,” leaving you with a burning or stinging sensation, explains Dr. Houman.
Bonus not-so-fun fact: less urine output also means bacteria aren’t flushed out as well, raising your chances of—you guessed it—a UTI, adds Dr. Houman. So if your pee is dark and painful, your body may just be begging for more water.
Urologic procedures
Had a recent urologic surgery or procedure? That burning sensation might not be an infection—it could just be irritation from the intervention itself. Anytime you tinker with the urethra, bladder, or ureter, stinging urination can follow.
Some possible triggers include:
- Double-J urinary stent: A thin, flexible tube with curled “J-shaped” ends, placed in the ureter to keep urine flowing from the kidney to the bladder (often after surgery or a kidney stone).
- Urethral instrumentation: When instruments are inserted into the urethra for diagnosis or treatment.
- Foley catheterization: A soft tube inserted into the bladder to drain urine.
Quick relief: what you can do now
When your pee feels like liquid fire, you want relief—fast. While these hacks won’t cure the cause, they can help calm the sting until you see a doctor.
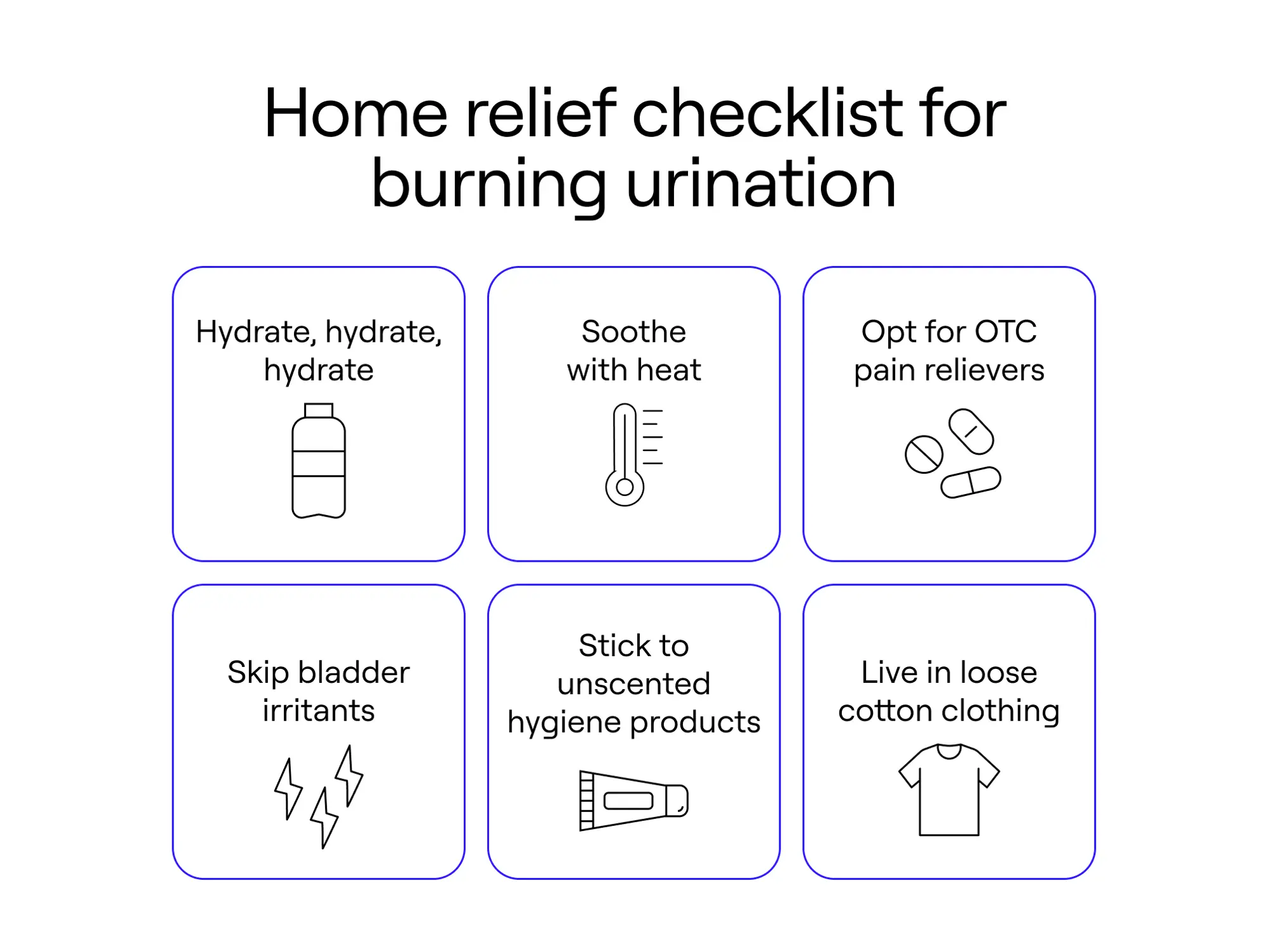
Home relief checklist for burning urination
Hydrate like it’s your job
“Best thing to do is hydrate,” says Dr. Houman. Why? Because water dilutes your urine, making it less acidic and less irritating when it hits an inflamed bladder. It also helps flush bacteria out of your urinary tract, so you’re not giving the germs a cozy home. Aim for steady sips all day rather than guzzling a gallon at once (your bladder will thank you).
Try OTC helpers
Over-the-counter painkillers like acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can take the edge off general discomfort. For bladder-specific relief, look for products with phenazopyridine (like Azo or Pyridium). They’re designed to quiet the constant burning and urgency, says Dr. Weinberg. Just a heads-up: they’ll turn your pee a startling shade of orange or red (don’t panic—it’s normal, he says). These are safe for short-term use, but don’t take them longer than a couple of days without talking to your doctor, since they only mask symptoms; they don’t fix the infection. Translation: You still need proper treatment from a doctor.
Soothe with heat
Sometimes your bladder pain feels more like a dull, crampy ache than a sharp burn. A heating pad on your lower belly—or a soak in a warm (not scalding) bath—can help relax tense muscles and calm that discomfort, says Dr. Weinberg. It’s like giving your bladder a mini spa day.
Skip the irritants
Coffee, alcohol, soda, spicy food, and acidic drinks (looking at you, OJ) can all poke at an already inflamed bladder, agree Drs. Houman and Weinberg. Save the hot wings and lattes for later. Right now, your bladder wants bland, boring, and easygoing.
Keep it gentle down there
When your urethra is already cranky, the last thing it needs is more irritation. Stick with fragrance free hygiene products, skip the harsh soaps or bubble baths, and choose loose, breathable clothing over tight jeans or synthetic underwear. Basically: let your bits breathe.
Don’t confuse relief with a cure
Important note: these quick fixes are Band-Aids, “not treatments for the underlying cause,” says Dr. Weinberg. “Quick relief shouldn’t replace medical evaluation, especially if symptoms persist beyond a day or two, or are severe,” adds Dr. Houman.
So, if the burn doesn’t back off quickly, or if you’re dealing with fever, back pain, or blood in your urine, call your doctor ASAP.
- Hydrate, hydrate, hydrate
- Soothe with heat
- Opt for OTC pain relievers
- Skip bladder irritants
- Stick to unscented hygiene products
- Live in loose cotton clothing
When to seek care (red flags)
A good rule of thumb: “always seek care if you have burning with urination, especially if it's new, persistent, or accompanied by other symptoms,” says Dr. Weinberg. “Don't try to tough it out or self-diagnose.”
According to Drs. Weinberg and Houman, seek care immediately if you notice:
- Fever or chills (possible kidney infection)
- Back or side pain (just below your ribs) (could be kidneys again)
- Nausea or vomiting and fever (likely a more serious infection)
- Blood in your urine (needs investigation to rule out serious conditions)
- Symptoms that don’t improve after a couple of days of home care (or that keep coming back)
- You’re pregnant (UTIs in pregnancy always need prompt treatment)
- Children or people assigned male at birth typically need additional evaluation, since infections are less common and may indicate an underlying issue.
- Weakened immune system (for example, due to diabetes, chemo, or certain meds) (infections can get serious, fast)
Moral of the story: If your pee feels like hot lava, and it’s not letting up, don’t wait it out. Get checked—your bladder (and your kidneys) will thank you.
A medical professional like those you can access virtually at General Medicine can help assess what’s going on, rule out anything serious, and guide you toward the right treatment that resolves your painful peeing ASAP.
How clinicians diagnose the cause
Figuring out what’s behind burning pee isn’t guesswork. Your provider has a toolbox of tests and exams to get to the bottom of it, from a simple urine dipstick to more advanced imaging if needed.
Medical history and physical exam
When it comes to figuring out why peeing feels painful, your story matters. Your provider will start by asking about your symptoms, medical history, and medications (since some meds can make conditions like BPH worse). Then comes the hands-on part:
- Prostate check (for people with prostates): A digital rectal exam (DRE) helps your doctor feel for a prostate that’s enlarged, tender, or otherwise irregular.
- Pelvic exam (for people with vaginas): Using a speculum, your provider looks for signs of vaginitis, like inflammation or discharge.
Urine tests
Urine doesn’t lie—and it’s often the first clue to what’s going on. There are several options for testing your pee:
- Dipstick test: Done in-office, this quick screen checks for white and red blood cells, protein, nitrites and leukocyte esterase (red flags for infection). Results are instant.
- Urinalysis: A more detailed lab test that counts white and red blood cells in your urine, usually ready in a few hours.
- Urine culture: The gold standard for diagnosing bladder or kidney infections. It reveals what bacteria are present and which antibiotic will work best. Results usually take 1–3 days.
Vaginal swabs and pH testing
If vaginitis is on the table, your provider may swab cervical or vaginal discharge for lab testing. They might also check your vaginal pH (higher pH can point to bacterial vaginosis or trichomoniasis). Just keep in mind—pH testing alone isn’t reliable, so it’s usually paired with other tests.
STI testing
Sometimes burning pee is an STI waving a big red flag. The type of test depends on your symptoms, sexual history, and what your provider finds in the exam. Samples might include:
- Blood (via draw or finger prick)
- Urine
- Swabs from the mouth, genitals, anus, or any sores/discharge (often self-collected)
For gonorrhea and chlamydia, the CDC recommends NAAT testing—a super-sensitive method that can use urine or swabs from the cervix, vagina, or urethra.
Imaging tests
When things seem more complicated (think: recurrent infections, blockages, flank pain, fever, or suspected stones/tumors), imaging may be in order:
- Ultrasound: Uses sound waves to get a picture of your organs.
- Computed tomography (aka CT scan): Uses X-rays to make cross-sectional images.
Most people with straightforward burning pee won’t need imaging, but it’s there if your case isn’t so simple.
Cystoscopy
If painful urination just won’t quit, your provider might suggest a cystoscopy. This quick procedure (5–10 minutes) uses a thin, flexible tube with a camera to peek inside your bladder and urethra. It’s helpful for spotting chronic issues such as stones, inflammation, or rarely, more serious conditions. You’ll get either numbing gel or anesthesia to keep things comfortable.
Treatments that actually work (by cause)
When it comes to stopping the sting, the fix depends on the cause. Here’s how to treat painful pee based on what’s really going on:
UTIs
Antibiotics are the gold standard here. Your provider will prescribe the right one, and symptoms usually ease within a couple of days. Just don’t ditch the meds early—finish the full course so the infection doesn’t boomerang back.
To ease the “ouch” while you wait for antibiotics to kick in, your provider may suggest phenazopyridine (Pyridium) or OTC versions like AZO, which help with burning, urgency, and frequency. Staying hydrated also helps flush bacteria out.
STIs
Painful pee can sometimes point to an STI, and treatments vary:
- Antibiotics (often a single dose) clear bacterial infections like gonorrhea, syphilis, chlamydia, and trichomoniasis.
- Antivirals can’t cure viruses like herpes or HIV, but they keep symptoms in check and reduce transmission risk.
Pro tip: skip sex until at least seven days after finishing treatment (and until sores heal, if you have them). Partners should also be tested and treated so you’re not just passing the infection back and forth.
Vaginitis
Vaginitis comes in different flavors, so treatment targets the cause:
- Bacterial vaginosis: antibiotics (oral or topical).
- Yeast infections: OTC antifungal creams or suppositories (like Monistat) or a prescription pill (fluconazole).
- Trichomoniasis: oral antibiotics such as metronidazole.
- Genitourinary syndrome of menopause (vaginal atrophy): estrogen therapy (creams, rings, or tablets).
- Noninfectious vaginitis: identify and ditch the irritant (new soap, detergent, pads, tampons, etc.).
Prostate problems
The root cause determines the treatment for a troublesome prostate:
- Prostatitis: antibiotics (if caused by a bacterial infection) and alpha-blockers (to relax the bladder neck and ease pain/flow).
- BPH (enlarged prostate):
- Lifestyle tweaks (less late-night drinking, cut caffeine/alcohol, manage constipation)
- Meds to shrink the prostate or relax muscles for better urine flow.
- Severe cases may need procedures or surgery to widen or remove part of the prostate.
Kidney stones
When it comes to stones, size matters. Here’s how they’re treated:
- Small stones: lots of water, pain relievers (ibuprofen/naproxen), and sometimes alpha-blockers to relax the ureter so the stone slips out more easily.
- Bigger stones: more intensive help may be needed, like:
- Shock wave therapy (ESWL) to break stones into passable pieces.
- Ureteroscopy (tiny camera and tools inserted through the bladder to snag or zap stones).
- Percutaneous nephrolithotomy (surgical removal through a small incision).
Cystitis
Treatment isn’t a one-size-fits-all for cystitis.
- Bacterial cystitis: antibiotics are the first line.
- Interstitial cystitis (bladder pain syndrome): trickier to treat. Options include oral meds, bladder instillations, nerve stimulation, pelvic floor PT, and sometimes diet changes (some people find relief by cutting caffeine, alcohol, tomatoes, chocolate, or spicy foods). Surgery is rare and reserved for a last resort. Because interstitial cystitis is complex and long-term, treatment is best guided by a urologist.
- Cystitis caused by chemical irritants: avoid the triggers (bubble baths, spermicides, perfumed products). Drink more water to help flush things out.
Standout box: No matter the cause of painful pee, don’t just grit your teeth and hope it passes. The right diagnosis = the right treatment = way less bathroom drama.
Prevention tips to reduce recurrence
You can’t dodge every cause of discomfort when urinating, but smart daily habits can lower your risk (and save you from repeat bathroom misery). Tried-and-true tips from Drs. Houman and Weinberg:
Hydrate like a champ. Water is your bladder’s best defense—it literally flushes bacteria out before they can settle in and cause trouble.
Keep it clean (but gentle). Hygiene matters: Wipe front to back, while uncircumcised men should retract the foreskin and wash gently. Skip the harsh soaps and scented products—they irritate more than they help. Stick to mild, fragrance-free options.
Pee after sex. It’s not glamorous, but it’s one of the easiest ways to flush bacteria out of the urethra after intercourse.
Don’t hold it in. When your bladder says “go,” listen. Holding it gives bacteria time to multiply, upping your risk of infection.
Dress for success. Cotton undies and loose clothes let things breathe, keeping the area dry and less friendly to bacteria. Tight, synthetic fabrics? Not your friend here.
Consider cranberry—but don’t count on it. Some studies show cranberry juice or supplements may make it harder for bacteria to stick to the bladder wall, but the science is mixed. Think “possible helper,” not cure-all. Some people find cranberry helpful, but it should never replace medical evaluation or treatment.
Manage what’s under the surface. Conditions like kidney stones, diabetes, enlarged prostate, or post-menopausal vaginal changes can all make infections more likely. Staying on top of these with your doctor lowers your risk.
Sometimes, even your best prevention game isn’t enough. If you’ve had 2 UTIs in 6 months or 3 in a year, you fall into the “recurrent UTI” category. In that case, doctors may suggest extra strategies, such as:
- Probiotics, D-mannose, and cranberry products (may help, though evidence is still up in the air).
- Topical estrogen for postmenopausal people, which can reduce recurrences.
- Prophylactic antibiotics as a last resort when nothing else works.
Special considerations
Burning pee isn’t one-size-fits-all—the way it shows up (and how doctors treat it) can vary a lot depending on age and gender. Here’s how the approach shifts in different groups:
Pregnant people
During pregnancy, UTIs are more than just annoying—they can be risky. Even bacteria in the urine without symptoms (asymptomatic bacteriuria) usually gets treated, since it can lead to kidney infections, premature labor, or low birth weight, says Dr. Weinberg. Diagnosis often involves a urine culture, and antibiotics are carefully chosen to ensure safety for both the pregnant person and the baby.
Men
UTIs in those assigned male at birth aren’t nearly as common, so when they do happen, doctors look deeper. Burning urination can point to issues like an enlarged prostate (BPH), kidney stones, STIs, or structural problems, says Dr. Houman. That’s why evaluation often includes prostate exams, imaging, or other specialized tests to nail down the real culprit.
Older adults
In older adults, UTIs don’t always look textbook. Instead of burning, symptoms may show up as incontinence, confusion, weakness, falls, or just feeling “off,” says Dr. Weinberg. Fever may be mild or missing altogether. With weaker immune systems and bladder-emptying issues (like BPH in men), UTIs are more common and more dangerous in this age group, sometimes leading to sepsis if untreated, he says. Doctors must carefully weigh kidney function and medication interactions when choosing treatment, adds Dr. Houman.
Children
For kids, painful urination is never something to brush off. Little ones often can’t explain their symptoms, so red flags might include fever, irritability, poor feeding, or foul-smelling urine, says Dr. Weinberg. Untreated UTIs can damage developing kidneys, especially if there’s a condition like vesicoureteral reflux (when urine flows backward), he says. Diagnosis usually requires a clean-catch urine sample (or catheterization in young kids), and treatment is key. After a first UTI, doctors often check for anatomical issues to prevent repeat infections.
The bottom line
Your urinary health is too important to ignore. That burning sensation may seem like no big deal, but if it’s brushed off, it can snowball into bigger problems—like an infection reaching your kidneys. In other words: don’t tough it out. Always get checked if symptoms persist, worsen, or come with red flags like nausea, fever, or flank pain.
The good news? Most causes are highly treatable once you know what you’re dealing with. Connect with a General Medicine clinician over video, right from your couch, to discuss your symptoms. You’ll get a personalized plan—whether that’s a prescription, lab work, or a referral for more complex issues—so you can put the fire out for good.
Key takeaways
- Burning pee isn’t a diagnosis—it’s a symptom, and causes range from infections to irritants to kidney stones.
- Quick fixes (like water, OTC pain relievers, or a heating pad) can ease the sting but won’t cure the root problem.
- Seek care fast if symptoms come with fever, blood in your urine, back pain, or if you’re pregnant.
- Prevention basics—hydration, hygiene, peeing after sex, and avoiding harsh products—can help cut your risk.
- Most causes are treatable, but the key is timely diagnosis and the right treatment plan.
General Medicine follows a strict editorial process, including using real experts to write our articles, vetted primary sources, fact-checking, a secondary medical review, and updates as necessary. This article was medically reviewed and fact checked by Swapna Ghanta, MD and Ecler Ercole Jaqua, MD.
FAQs
How do I get rid of the burning sensation after I pee?
It depends on what’s causing it. “Burning with urination is a symptom, not a diagnosis,” says Dr. Houman. Infections, kidney stones, dehydration, chemical irritants, even prostate or bladder issues could be behind it. The bottom line: don’t ignore it, especially if it keeps happening or comes with other red-flag symptoms. Most causes are very treatable, but catching it early helps you avoid bigger problems, he says.
Why does my pee burn if I don’t have an infection?
Not every burning pee is a UTI or STI. Other culprits include bladder inflammation, kidney stones, an enlarged prostate, vaginal atrophy, or even something as simple as a new soap or bubble bath. Since the causes vary so widely, it’s worth getting checked out so you can rule out anything serious and land on the right treatment.
How can I soothe that “pee burn” feeling?
While only a doctor can fix the root cause, these tips –courtesy of Drs. Weinberg and Houman– can help soothe the sting in the meantime:
- Hydrate: Water dilutes your urine, making it less harsh and helping flush out bacteria.
- Try OTC meds: Acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) ease general pain. For targeted bladder relief, phenazopyridine (Azo, Pyridium) can quiet burning and urgency.
- Bring the heat: A warm bath or heating pad on your lower belly can relax cramps and soothe bladder pain.
- Skip irritants: Coffee, alcohol, spicy foods, and acidic drinks can make things worse.
- Keep it gentle: Stick to fragrance-free hygiene products and loose clothing to avoid extra irritation.
What medication actually stops the burn?
Over-the-counter pain relievers (Tylenol, Advil, Motrin) can take the edge off while products with phenazopyridine (Azo, Pyridium) can calm burning and urgency.
Don’t panic if phenazopyridine turns your pee bright orange or red (it’s normal). Just remember, these meds only mask symptoms. If you’ve got an infection, you’ll still need antibiotics or other prescriptions from your doctor to actually fix the problem.
Can dehydration really cause burning pee?
Yep! Think of it this way: your kidneys filter out waste and salts, and water dilutes all that into urine, says Dr. Weinberg. If you’re low on fluids, your pee becomes super concentrated—basically, a harsher chemical cocktail sliding through your urethra. “It’s less like a gentle rinse and more like a stronger, abrasive wash,” he says. That can irritate the delicate lining of your urinary tract and cause stinging.
Staying well-hydrated keeps your urine gentle, keeps things flowing, and helps flush out irritants or bacteria before they can cause trouble.
Our editorial standards
At General Medicine, we cut through the clutter to make health care clearer, faster, and easier to navigate. Every article is grounded in evidence-based research and peer-reviewed journals, reviewed by medical professionals, and written in accessible language that helps you make health decisions with confidence. We’re committed to ensuring the quality and trustworthiness of our content and editorial process by providing information that is up-to-date, accurate, and actually useful. For more details on our editorial process, see here.




