Jump to
Book a visit
$25 typical copay
$100 without insurance
Get expert care for your pain today.
Ugh, the itch! Poison ivy can sneak up on you, but it doesn’t have to win. The trick is speed: Wash off the oil ASAP, then lean on old-school fixes like calamine, oatmeal baths, and hydrocortisone to keep the itch from driving you up the wall. And remember: Once the oil’s gone, you can’t “spread” the rash, no matter how scary the blisters look. Most cases are just uncomfortable, but if the rash hits sensitive spots like your eyes or causes major swelling, it’s worth urgent medical attention. Otherwise, stop stressing about contagion, focus on feeling human again, and start to give those “leaves of three” the side-eye they deserve.
If you’ve ever spent a summer afternoon pulling weeds, clearing a trail, or chasing kids through a patch of tall grass, you may have met one of the great outdoor equalizers: poison ivy. One careless brush against its leaves can leave you with an itchy, blistering rash that feels wildly out of proportion to the innocent-looking plant, making it all the more important to know how to treat poison ivy quickly and effectively.
Here’s what’s happening: Poison ivy, poison oak, and poison sumac all produce an oily resin called urushiol. It only takes a microscopic amount—literally less than a grain of salt—to trigger a reaction in most people. That means leaning against a vine, petting a dog that rolled in the brush, or even picking up a contaminated tool can be enough to set things off.
Once on the skin, urushiol sinks in fast. Unless you wash it away within minutes, your immune system will flag it as a threat and respond with red, swollen, and incredibly itchy skin. This reaction is called a “type IV delayed hypersensitivity response,” and is why new patches of rash can appear over several days after the initial exposure.
“A poison ivy rash usually appears within 12 to 48 hours after contact with urushiol,” says Hannah Kopelman, MD, a dermatologist at DermonDemand. “The rash itself can last anywhere from one to three weeks, depending on the severity and whether treatment is started early.”
And poison ivy doesn’t discriminate. Whether you’re a seasoned backpacker, a casual gardener, or a kid building a fort in the woods, you’re at risk if you spend time outdoors. About 90% of people are sensitive to urushiol, and each year, as many as 50 million Americans develop poison ivy rashes. While most cases are mild, they’re almost always uncomfortable—and sometimes severe enough to need prescription treatment.
The upside: Once you understand the plant, the rash, and the steps that actually help, you can take control. This guide covers everything you need to know about how to treat poison ivy, from immediate first aid and effective home remedies to prevention tips and the red flags that mean it’s time to see a doctor. Think of it as your poison ivy survival playbook, so the next time your weekend hike turns into an itchy misadventure, you’ll know exactly what to do.
Spotting the rash (and when it’s NOT contagious)
Poison ivy doesn’t usually show up right away. At first, you might just feel a little itch or see faint redness. Then, like clockwork, it escalates into one of the itchiest rashes you’ll ever experience.
Poison ivy first aid
Classic signs include:
- Redness and swelling in the area that touched the plant
- Clusters or streaks of blisters (often forming a straight or curved line, tracing where the leaves brushed your skin)
- Severe itching
- Oozing or crusting in areas where blisters break open
In other words, if you’ve ever wanted to crawl out of your own skin, poison ivy will happily provide that experience.
But here’s the good news: The fluid inside the blisters does not spread the rash, says Rosanne Paul, DO, assistant professor of dermatology at Case Western Reserve University.
“What actually causes spread is lingering urushiol on the skin, clothing, shoes, tools, or even pet fur. If that resin is not washed off, you can keep re-exposing yourself or others,” explains Kopelman. “Once the oil is gone, the rash itself is not contagious.”
This distinction matters because it takes away a lot of anxiety. Once you’ve washed your skin, nails, and gear thoroughly, you won’t “give” poison ivy to others just by being around them, says Paul. The rash may look angry, but it’s your body’s immune system reacting—not something contagious like chickenpox.
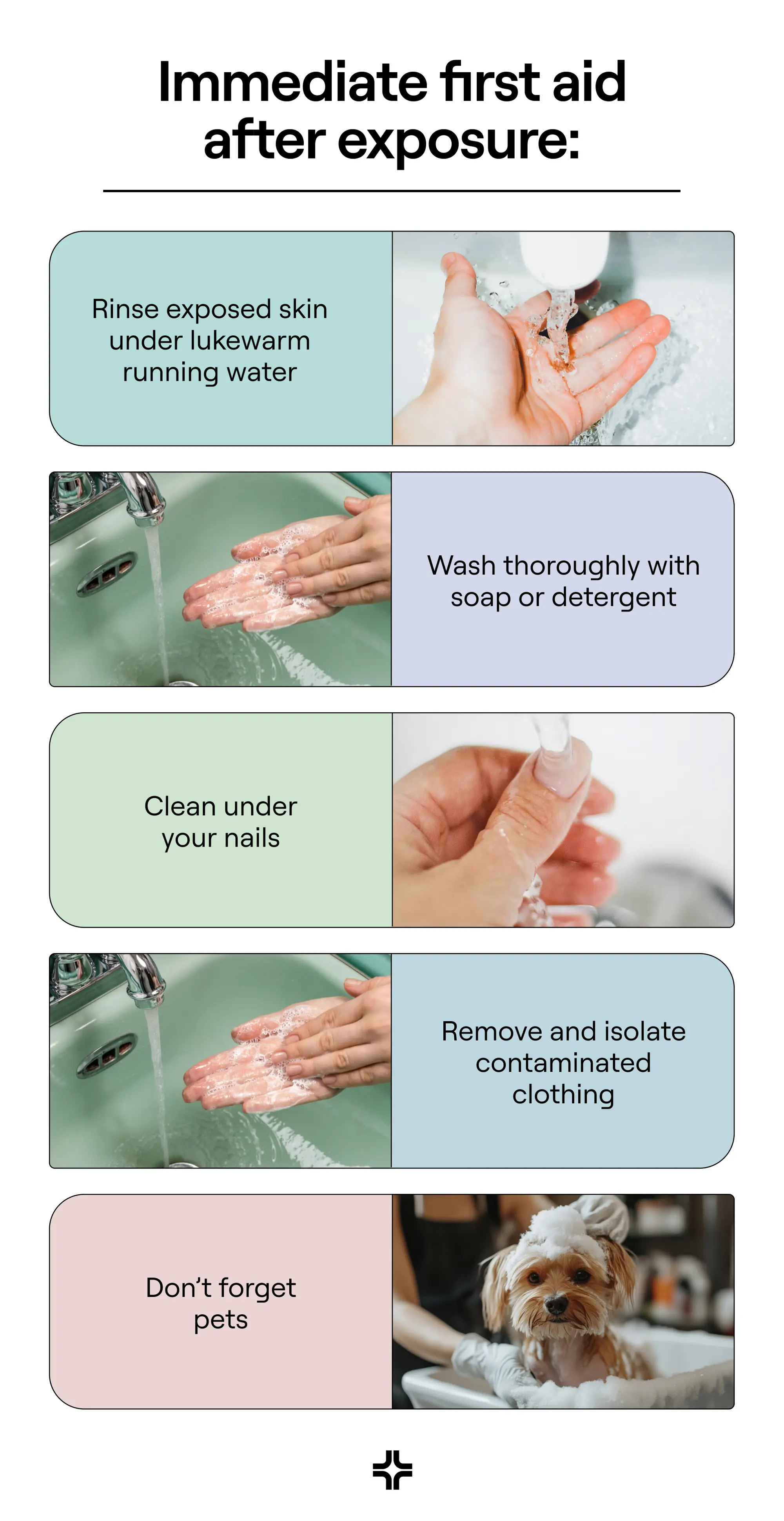
Immediate first aid after exposure (minutes to hours)
When it comes to poison ivy, timing really is everything. Urushiol sticks to skin fast, but Kopelman says that washing the skin within the first 10–15 minutes—and ideally no later than 30 minutes—gives you the best chance to prevent or significantly reduce the rash. Think of it like a race: you versus urushiol. The sooner you move, the better your odds.
Here’s your playbook for immediate care:
- Rinse exposed skin under lukewarm running water: Skip hot water—it opens pores and can actually help the oil sink in deeper. And don’t stand in a bathtub where the oil can spread around. Running water is best.
- Wash thoroughly with soap or detergent: Regular dish soap works just fine, but specialty cleansers like Tecnu or Zanfel are designed to break down urushiol more effectively. The key is to wash gently but thoroughly—no need to scrub your skin raw. And resist the urge to reach for harsh solvents or bleach. Alcohol, gasoline, and bleach won’t “neutralize” urushiol; they’ll just damage your skin and leave you with a bigger problem.
- Clean under your nails: Urushiol loves to hide under fingernails, which means every absentminded scratch risks redepositing it somewhere else. A quick nail brush or even a soapy toothbrush does the trick. Make sure you wash any tools thoroughly after using them.
- Remove and isolate contaminated clothing: Toss clothes, towels, or gloves into a plastic bag until you can wash them separately in hot water with detergent. Urushiol can stay active on fabrics for months.
- Don’t forget pets: Dogs and cats don’t react to urushiol, but their fur can carry it like a shuttle bus straight to your skin. Give them a bath (ideally with gloves on) if you suspect they’ve rolled through the plants.
Pro tip: Have a post-yardwork routine. If you garden, hike, or do landscaping regularly, make a habit of showering and changing clothes right after. It’s not glamorous, but it’s one of the most effective poison ivy treatments there is (because prevention beats weeks of itching every time).
Home remedies & self-care (mild to moderate rash)
Once the rash has set in, your goal shifts from “get the oil off” to “make the itch bearable and let your skin heal.” According to Paul and Kopelman, these home remedies for poison ivy can help you stay sane while your immune system does the heavy lifting:
- Cool compresses: A clean washcloth soaked in cool water and pressed on the rash for 15 to 20 minutes can calm the fire temporarily. Stash a damp cloth in the fridge so it’s ready when the itch kicks up.
- Colloidal oatmeal or baking soda baths: Oatmeal baths coat the skin in a soothing film that takes the edge off itching. Baking soda works similarly by balancing pH and calming irritation.
- Calamine lotion or zinc oxide: These chalky pink and white classics are still around for a reason: they help dry oozing spots and soothe raw skin. Not pretty, but effective.
- Topical corticosteroids: A low-strength steroid cream (like over-the-counter hydrocortisone) can reduce inflammation.
- Oral pain relievers: Ibuprofen or acetaminophen can take the edge off if swelling or discomfort keeps you up.
- Sedating antihistamines at night: Even though histamine isn’t the main driver of poison ivy itch, meds like diphenhydramine (Benadryl) can help you sleep when scratching is relentless.
These skincare habits can also make the difference between a rash that heals smoothly and one that lingers or gets infected:
- Do keep nails short: Scratching is hard to resist, but shorter nails reduce the damage if you cave. Short nails also make it harder for stray urushiol to hide under your fingertips and spread to other patches of skin.
- Do wear loose, breathable clothing: Tight fabrics trap heat and sweat, which only ramps up the itch.
- Don’t scratch or pop blisters: It won’t speed healing, and it opens the door to bacteria.
- Don’t layer on random creams: Sometimes “more” just means “more irritation.” Stick to the basics above.
Some treatments that sound promising may actually do more harm than good. These over-the-counter products are notorious for causing allergic skin reactions of their own—basically trading one rash for another. Consider speaking to a provider before using, especially if you have had a prior reaction to the below :
- Topical antihistamines like topical diphenhydramine (Benadryl cream)
- Benzocaine (a numbing agent)
- Neomycin (an antibiotic in triple-ointment mixes)
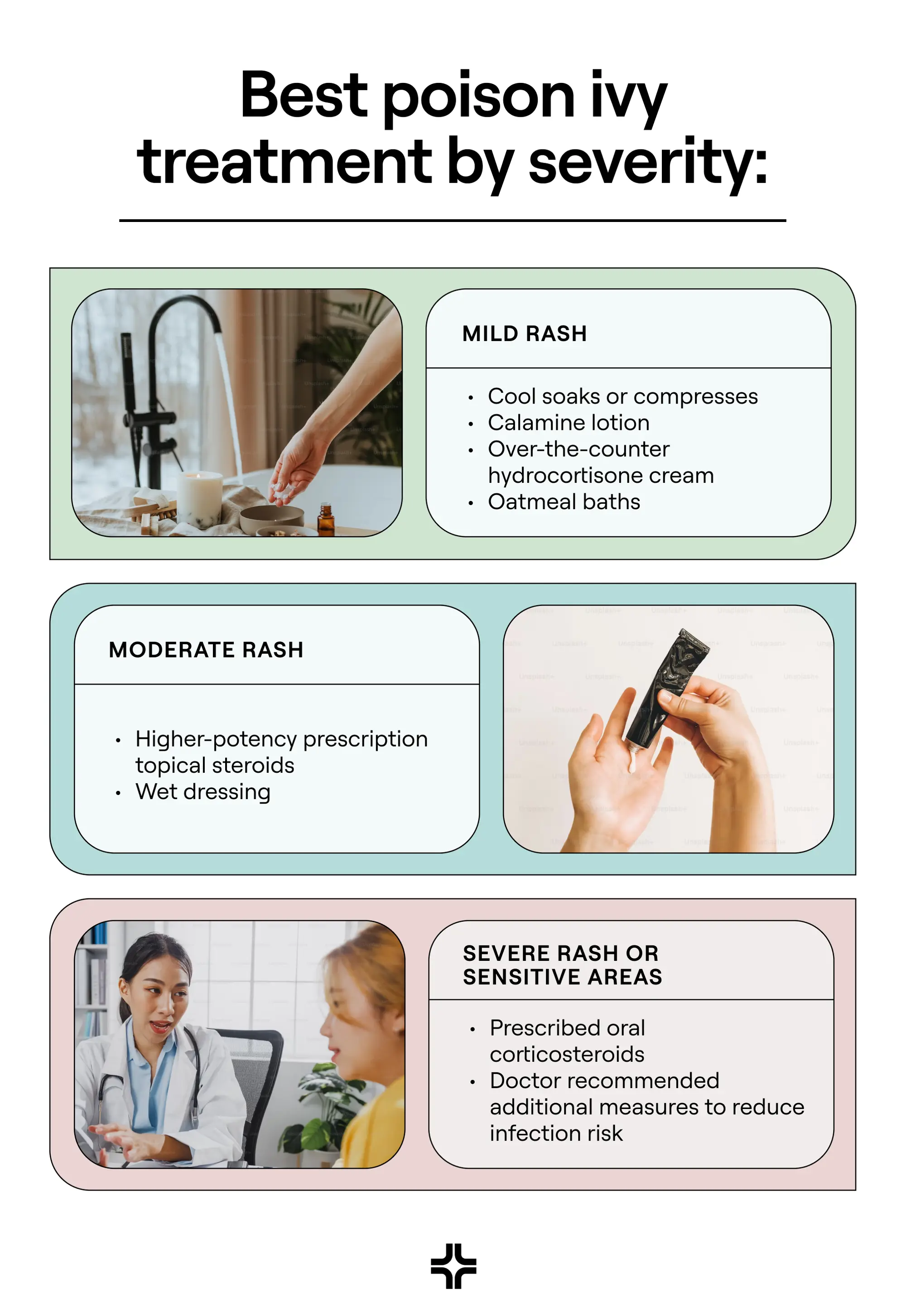
Best poison ivy treatment by severity (what actually works)
Not every poison ivy rash is created equal. Some patches are a mild nuisance you can manage with an oatmeal bath, while others demand a trip to the doctor for prescription meds. The best treatment depends on where the rash is, how much skin is involved, and how you feel.
Poison ivy treatment by severity
Mild rash
For localized, limited itch from everyday backyard brush, Raj Dasgupta, MD, a board-certified internal medicine doctor and medical advisor for Sleepopolis, recommends simple comfort care:
- Cool soaks or compresses
- Calamine lotion
- Over-the-counter hydrocortisone cream
- Oatmeal baths
Moderate rash
If the rash is spreading across several body parts, or the swelling or oozing makes you feel like a human tree sap experiment, it may be time to bring in stronger tools. Dasgupta suggests:
- Higher-potency prescription topical steroids to relieve inflammation, carefully monitored by a clinician
- Wet dressings like Burow’s solution, which cools inflammation and helps dry out blisters
Severe rash or sensitive areas
This is where poison ivy stops being an annoyance and starts interfering with daily life.
“Severe cases—especially if they involve the face, genitals, or large areas, or if there is significant swelling or blistering—need prompt medical attention,” says Dasgupta.
Fortunately, there are treatment options that could help prevent the rash from worsening and shorten its course. They include:
- Oral corticosteroids are the gold standard and must be prescribed as a two- to three-week taper. Short bursts without a taper can lead to “rebound” dermatitis, which is when the rash comes roaring back worse than before.
- Your doctor may recommend additional measures to reduce infection risk (like keeping blisters covered) or medication to help you sleep through the itch.
In the case of a severe rash, you also need to keep an eye out for a potential secondary infection. These signs mean bacteria have moved into your body, and you’ll likely need an oral antibiotic prescribed by a clinician:
- Increasing pain
- Yellow crust or pus
- Spreading redness
- Fever
When to see a doctor (red flags)
Most poison ivy rashes are annoying but self-limited. Still, there are times when toughing it out isn’t the right call. According to Kopelman, if you notice any of these red flags, it’s time to trade the calamine lotion for professional care:
- Rash in sensitive areas: Poison ivy on the face, eyelids, or genitals can interfere with vision, urination, or daily activities. Swelling in these areas can escalate quickly and should be evaluated by a clinician.
- Extensive blistering: If large portions of your body are covered or the blisters are so widespread you can’t comfortably sleep or drink fluids, that’s beyond home-remedy territory.
- Signs of infection: Redness spreading beyond the rash, increasing warmth, pus, crusting, or fever are signs bacteria has joined the party. You’ll likely need antibiotics to clear it.
- Higher-risk groups, including babies, pregnant people, and anyone who is immunocompromised should contact their healthcare provider promptly for individualized treatment, even if the rash seems mild. What’s a nuisance rash in most people can become more serious in these groups.
Certain scenarios require immediate medical care. “If someone has trouble breathing or swallowing after exposure, that is an emergency, and they should go to the ER right away,” says Kopelman.
How clinicians diagnose & treat
Poison ivy announces itself loud and clear, so doctors can usually diagnose it by sight. They’ll also ask about your recent activities and look at the pattern of your rash. Those classic streaky lines or clusters of blisters are usually enough to clinch the diagnosis.
From there, treatment depends on how severe things are:
- Prescription-strength topical steroids: For moderate cases, your doctor may prescribe a more potent steroid cream or ointment than what you can buy at the drugstore. These reduce inflammation and help calm itching faster.
- Systemic (oral) steroids: For severe reactions, oral steroids like prednisone are the go-to.
- Short-term antipruritics: Medications to ease itching or help you sleep may be offered as a temporary assist.
- Wound care: If blisters are open or raw, your clinician may suggest dressings, wet wraps, or ointments to prevent infection.
Finally, most clinicians won’t let you leave without a little poison ivy prevention counseling. Expect advice on how to avoid re-exposure, how long urushiol can linger on gear, and why it’s worth laundering those yardwork clothes twice.
How to get rid of poison ivy (from your environment)
Treating your rash is only half the battle. If poison ivy is thriving in your yard or along a favorite trail, you’ll keep running into it (literally) until it’s gone. Here’s how to safely evict the plant without giving yourself a repeat rash in the process.
- Suit up before removal: Urushiol doesn’t care how tough you are; it will get you if your skin is exposed. Before pulling plants, put on gloves (preferably vinyl, as urushiol can seep through thin latex), long-sleeve pants and shirts, and closed shoes. When in doubt, dress like you’re heading into battle.
- Remove the plant, roots and all: Poison ivy spreads through underground rhizomes, so clipping the top is just like a haircut—it’ll grow back. Dig out the whole plant, seal it in a heavy-duty trash bag, and never compost it (urushiol doesn’t break down easily). For large infestations, consider a professional removal service—sometimes outsourcing is the safest (and least itchy) option.
- Never burn poison ivy: It might be tempting to toss it on the burn pile, but this is a hard no. Burning poison ivy releases urushiol into the smoke, and inhaling it can cause severe, life-threatening lung inflammation. This is an ER-level emergency, not a backyard cleanup. Stick to bagging and trash disposal.
- Decontaminate everything: Urushiol is stubborn. It can remain active on surfaces for months—even years—if not washed away. After removal, wash tools, boots, and gloves with soap and hot water, wipe down hard surfaces, and don’t forget pet leashes or toys.
Prevention 101
The best poison ivy rash treatment is never needing one in the first place. While you can’t control where the plants grow, you can stack the odds in your favor with a few simple prevention habits.
First, learn to spot it. You’ve probably heard the rhyme: “Leaves of three, let it be.” Poison ivy and oak usually have clusters of three leaflets, while poison sumac sports clusters of seven to 13.
The catch? These plants don’t always look the same—leaves can be shiny or dull, green in spring, red in fall, or even a bit fuzzy depending on the species and region. If you spend a lot of time outdoors, look up photos of the specific plants common where you live so you can ID them on sight.
Protecting your skin is also half the battle. Wear long sleeves, pants, gloves, and boots to create a simple but effective shield. It may not win you style points, but it will help you walk away from the backyard itch-free. Barrier creams with bentoquatam (like IvyBlock) add another layer of defense—apply them at least 15 minutes before potential exposure and reapply as directed.
And even if you don’t think you touched poison ivy, make it a routine to clean up after any potential exposure.
Quick prevention recap:
- Wash your skin promptly with soap and lukewarm water.
- Launder clothes separately in hot water to remove urushiol from fabrics.
- Rinse gear, tools, and pet fur thoroughly—urushiol can linger for months.
- Wear protective clothing and apply barrier creams before outdoor activity.
Special situations & look-alikes
Not every itchy rash in summer is poison ivy: Sometimes, your skin can react to things you wouldn’t expect. That’s because urushiol belongs to a family of plant chemicals that show up in surprising places. If you’re sensitive to poison ivy, you may also react to:
- Mango rind: The peel—not the fruit—can cause the same blistery rash if you handle it unpeeled.
- Cashew shells: Raw cashews have a similar oil in their shells (which is why the ones you buy are always pre-processed).
- Ginkgo fruit hulls: Handling ginkgo fruit can sometimes cause a poison ivy–like rash.
Poison ivy is so common that it often gets blamed for any mysterious rash. But if yours doesn’t follow the usual timeline or have the classic streaky, blistery look, it’s time for a second opinion. A clinician can help determine if it’s truly poison ivy or another skin condition that looks similar, such as:
- Scabies: Caused by tiny mites burrowing in the skin, scabies leads to intense itching (especially at night) and can look like small, red bumps or tracks.
- Shingles: This painful rash, caused by a reactivation of the chickenpox virus, usually appears in a stripe or patch on one side of the body, not in random streaks.
- Cellulitis: This bacterial skin infection causes spreading redness, warmth, and swelling. Unlike poison ivy, it’s often tender or painful rather than just itchy.
- Other contact dermatitis: Soaps, cosmetics, or nickel jewelry can cause allergic rashes that resemble poison ivy but don’t follow the “leaves of three” storyline.
If your rash doesn’t match the usual streaky pattern or timeline, see a clinician to confirm the diagnosis and rule out other skin conditions.
The takeaway
- Wash skin, nails, clothes, gear, and even pets quickly after possible exposure—urushiol is stubborn but beatable.
- Blisters may look dramatic, but the fluid inside doesn’t spread the rash. Lingering urushiol does.
- Mild rashes usually respond to cool compresses, oatmeal baths, calamine, and hydrocortisone.
- If your rash spreads to your face, eyes, or genitals, covers more than 20% of your body, or shows signs of infection, those are signs that it’s time to see a doctor.
- Severe cases often need oral steroids—don’t tough it out if you can’t sleep, eat, or function.
- Prevention is your best friend: Learn to spot the plant, cover up, and clean up after outdoor time.
Frequently Asked Questions (FAQs)
What not to put on a poison ivy rash?
It’s best to skip topical antihistamines like Benadryl cream, benzocaine, and triple-antibiotic ointments with neomycin—as they can cause allergic reactions of their own and worsen the rash. Also, skip harsh scrubbing, bleach, and alcohol, which damage your skin without helping.
What clears up poison ivy the fastest?
The fastest way to stop poison ivy in its tracks is to wash exposed skin with soap and lukewarm water within 30 minutes of contact. If the rash has already developed, nothing makes it disappear overnight, but calamine lotion, oatmeal baths, cool compresses, and hydrocortisone cream can ease symptoms and speed healing. Severe cases may need prescription steroids from a doctor.
How to make poison ivy stop spreading?
Once you’ve washed the urushiol oil from your skin, nails, clothes, pets, and gear, the rash can’t spread. “New” patches popping up later are usually a delayed reaction or re-exposure to contaminated items, not the blisters themselves spreading.
How to treat poison ivy while pregnant?
Stick with the safest basics: cool compresses, oatmeal baths, calamine lotion, and breathable clothing. Low-strength hydrocortisone cream may be used under a doctor’s guidance. More aggressive treatments, like oral steroids, are only used in severe cases where the benefits outweigh the risks, so always talk to your OB or dermatologist first.
How long does poison ivy last to go away?
Most rashes last one to three weeks. With proper care—and medical treatment if needed—you can speed recovery and avoid complications.
General Medicine follows a strict editorial process, including using real experts to write our articles, vetted primary sources, fact-checking, a secondary medical review, and updates as necessary. This article was medically reviewed and fact-checked by Swapna Ghanta, MD and Ecler Ercole Jaqua, MD.
Our editorial standards
At General Medicine, we cut through the clutter to make health care clearer, faster, and easier to navigate. Every article is grounded in evidence-based research and peer-reviewed journals, reviewed by medical professionals, and written in accessible language that helps you make health decisions with confidence. We’re committed to ensuring the quality and trustworthiness of our content and editorial process by providing information that is up-to-date, accurate, and actually useful. For more details on our editorial process, see here.




